In a groundbreaking advancement that holds promise for the future of oncology, researchers at the University of Sharjah have unveiled pioneering insights into the application of artificial intelligence (AI) for the early detection and management of pancreatic cancer. This lethal malignancy, often diagnosed at an advanced stage due to subtle or absent early symptoms, poses formidable challenges that have long hindered effective intervention. The study, recently published in the Beni-Suef University Journal of Basic and Applied Sciences, rigorously explores how AI technologies, particularly those leveraged in image analysis and multiomics integration, could fundamentally transform prognosis, diagnosis, and personalized treatment plans for pancreatic cancer patients.
The research delineates AI’s multifaceted role across several stages of pancreatic cancer management. From refining image-based diagnostics to predicting therapeutic responses, AI models exhibit remarkable potential in enhancing clinical decision-making. Through advances in machine learning and deep neural networks, computational systems are now capable of parsing complex biomedical data sets, including radiographic images, genomic profiles, and proteomic patterns, with unprecedented accuracy and speed. These capabilities enable clinicians to detect subtle abnormalities indicative of nascent tumors, which are often imperceptible to human observers.
.adsslot_sbAndpK4al{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_sbAndpK4al{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_sbAndpK4al{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
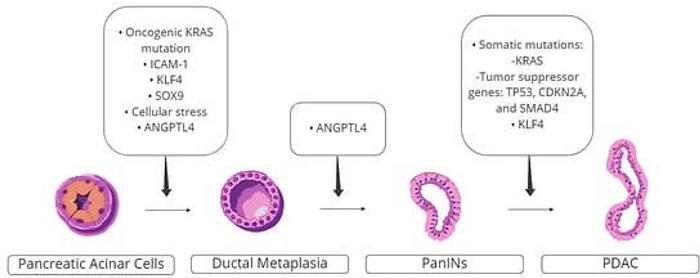
One of the most transformative aspects reviewed in this study is the integration of multiomics data—comprehensive analytical approaches that synergize genomic, transcriptomic, proteomic, and metabolomic information into cohesive predictive models. AI algorithms decipher these multi-layered biological datasets to elucidate intricate disease pathways and mutation landscapes that drive pancreatic tumorigenesis. The ability to amalgamate heterogeneous data sources empowers personalized medicine approaches, tailoring treatments based on individual molecular profiles and predicted disease trajectories.
Despite this promise, the researchers caution that AI adoption in clinical settings is hampered by interpretability challenges. The “black box” nature of many AI algorithms creates obstacles in understanding how conclusions are derived, often leaving clinicians skeptical of their outputs. This opacity can limit trust in AI recommendations, thereby impeding broader clinical integration. To address this, the field is witnessing an upsurge in the development of explainable AI methods, which endeavor to produce transparent and interpretable results through visualization tools, feature relevance scores, and natural language explanations.
Explainable AI stands to democratize advanced computational tools, bridging the gap between data scientists and healthcare practitioners. By making AI decisions comprehensible and actionable, it fosters a collaborative environment where clinicians can critically evaluate algorithmic predictions and integrate them confidently into treatment planning. This paradigm shift is expected to accelerate the transition of AI from experimental frameworks into routine clinical workflows, thereby enhancing patient outcomes.
Machine learning models have demonstrated a high sensitivity in detecting pancreatic neoplasms at an early stage, where intervention can drastically alter prognosis. These models not only assist in identifying tumors but also stratify patients according to risk profiles, guiding oncologists in selecting optimal therapeutic regimens. The study highlights successes in predicting patient responses to standard therapies—including chemotherapy, radiation, immunotherapy, and surgery—using AI-driven predictive analytics that analyze baseline patient data and tumor characteristics.
In addition to computational advances, the research points to the burgeoning role of the Internet of Things (IoT) within pancreatic cancer management. IoT-enabled devices facilitate continuous monitoring of patient health metrics, enabling real-time data collection that feeds into AI systems for dynamic risk assessment and treatment adjustment. Such technological integration promises to usher in an era of precision oncology, where interventions are continually refined based on the evolving physiological state of the patient.
Nonetheless, the deployment of AI tools requires careful governance and comprehensive understanding to mitigate risks associated with erroneous or biased outputs. Multidisciplinary collaboration among oncologists, data scientists, bioinformaticians, and healthcare administrators will be crucial to establish robust validation protocols, ethical standards, and practical guidelines for AI utilization in pancreatic oncology.
In conclusion, the study by the University of Sharjah researchers underscores the transformative potential of artificial intelligence in confronting one of the most formidable cancers confronting modern medicine. By harnessing the power of AI and integrating it with the vast complexity of multiomics data and IoT technologies, the medical community edges closer to an era of personalized, precise, and early pancreatic cancer intervention. Although challenges remain—principally in algorithmic transparency and clinical acceptance—the trajectory of AI in oncology signals an exciting frontier that could significantly reduce the morbidity and mortality associated with this devastating disease.
Subject of Research: Not applicable
Article Title: Advancing pancreatic cancer management: the role of artificial intelligence in diagnosis and therapy
News Publication Date: 7-Apr-2025
Web References:
https://link.springer.com/article/10.1186/s43088-025-00610-4
https://www.wcrf.org/preventing-cancer/cancer-statistics/pancreatic-cancer-statistics/
References:
Beni-Suef University Journal of Basic and Applied Sciences, 2025, DOI: 10.1186/s43088-025-00610-4
Image Credits: Current Oncology (2022)
Keywords: Diseases and disorders, Pancreatic cancer, Artificial Intelligence, Multiomics, Machine Learning, Explainable AI, Oncology, Internet of Things (IoT)
Tags: advancements in cancer researchAI in cancer detectionartificial intelligence in oncologychallenges in pancreatic cancer detectionearly-stage pancreatic cancer diagnosisimage analysis in medical researchleveraging AI for disease managementmolecular markers in pancreatic cancermultiomics integration in cancer treatmentpancreatic cancer prognosis predictionpersonalized treatment plans for cancerUniversity of Sharjah research on AI and cancer