In a breakthrough study poised to reshape therapeutic strategies for unresectable hepatocellular carcinoma (uHCC), researchers have identified distinct patterns in the behavior of alpha-fetoprotein (AFP) levels that independently predict patient outcomes under lenvatinib treatment. Hepatocellular carcinoma, a primary malignancy of the liver, presents significant clinical challenges when surgical resection is no longer an option. The dynamic monitoring of biomarkers, particularly AFP, offers a promising avenue to gauge treatment efficacy and improve survival prognostication, marking a crucial step forward in precision oncology.
Alpha-fetoprotein has long been utilized as a clinical biomarker in liver cancer diagnosis and surveillance. However, its dynamic changes over the course of systemic therapy remained underexplored until this latest retrospective, multicenter cohort study involving 553 uHCC patients treated with lenvatinib. Lenvatinib, a tyrosine kinase inhibitor with potent antiangiogenic properties, has gained approval as a first-line systemic agent for advanced HCC, but predicting which patients derive the greatest benefit has been elusive. This study uniquely applies advanced statistical modeling to AFP trajectories, offering nuanced insights beyond static measurement.
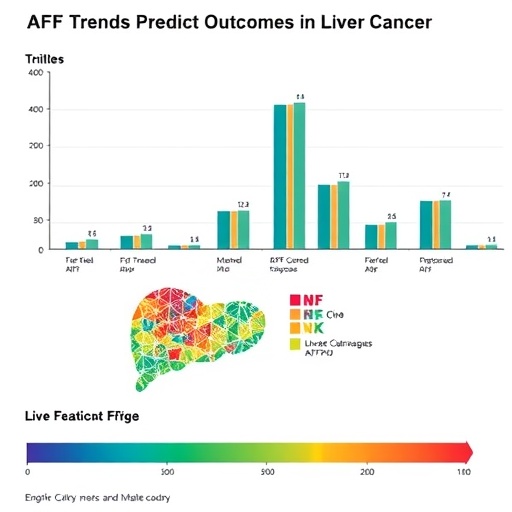
Utilizing a latent class linear mixed model—a sophisticated technique to capture underlying patterns within longitudinal data—the investigators classified AFP changes into four distinct trajectories: High-stable, High-rising, Sharp-falling, and Low-stable. Each trajectory represents a unique biological and clinical response pattern during lenvatinib treatment. This classification was grounded in analyzing serial AFP levels collected from patients across four oncology centers over three years, enhancing the robustness and generalizability of findings.
.adsslot_itPZJL1kxg{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_itPZJL1kxg{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_itPZJL1kxg{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Notably, the study revealed that patients exhibiting the Sharp-falling and Low-stable AFP trajectories experienced significantly improved overall survival (OS) and progression-free survival (PFS) compared to those with High-stable trajectories. Specifically, hazard ratios for mortality indicated a 72% and 58% reduction in risk for the Sharp-falling and Low-stable groups, respectively, marking a profound difference in prognosis associated with AFP dynamics. Similarly, the risk of disease progression diminished markedly within these groups, highlighting the AFP trajectory’s potential utility as a predictive biomarker.
Conversely, patients categorized under the High-rising trajectory did not demonstrate statistically significant survival benefits relative to the High-stable group, underscoring the importance of not only absolute AFP levels but their temporal patterns. These distinctions emphasize that a simple binary of high versus low AFP may insufficiently capture the biological complexity underlying treatment response, advocating for dynamic biomarker monitoring in clinical practice.
The clinical implications of these findings are manifold. First, encouraging longitudinal AFP monitoring could allow oncologists to stratify patients more effectively according to their anticipated response to lenvatinib. This stratification can inform adaptive treatment modifications, such as dose adjustments or the integration of complementary therapies in patients unlikely to respond favorably. Moreover, AFP trajectory analysis provides a non-invasive, cost-effective biomarker strategy, circumventing the need for more invasive or expensive modalities in routine follow-ups.
Beyond immediate clinical application, this research exemplifies the power of integrating advanced biostatistical methodologies into oncology studies. The latent class linear mixed model facilitated uncovering heterogeneity in treatment response hidden beneath aggregate data, pointing to the future of personalized medicine that utilizes computational techniques to identify subpopulations within heterogeneous diseases like HCC. This approach may be extended to other cancer biomarkers and therapeutic contexts, magnifying its translational potential.
Furthermore, the utilization of retrospective multicenter data spanning multiple years fortifies the reliability and clinical relevance of the study’s conclusions. Such collaboration across centers mitigates biases that might arise from smaller single-center cohorts and captures real-world patient diversity, which is critical for the applicability of predictive models in heterogeneous clinical settings. The study design also reflects the increasing embrace of big data analytics within oncology, a trend expected to accelerate in the coming years.
Despite these promising advancements, challenges remain in fully integrating AFP trajectory monitoring into routine clinical workflows. Standardization of AFP measurement intervals, inter-laboratory assay variability, and the need for real-time data analytics infrastructure are practical hurdles to be addressed. Nonetheless, the demonstrated prognostic power of AFP trajectories sets a compelling rationale for further prospective validation and health system integration.
Importantly, lenvatinib’s mechanism as a multikinase inhibitor, targeting VEGFR, FGFR, PDGFR, and others, intersects with tumor angiogenesis and cell proliferation pathways. The association between AFP dynamics and survival outcomes might reflect underlying tumor biology modulated by lenvatinib’s molecular effects. Future mechanistic studies could elucidate how AFP production correlates with tumor microenvironment alterations under systemic treatment, deepening understanding and enhancing biomarker-driven therapy.
Additionally, the absence of significant differences in outcomes for the High-rising group compared to the High-stable cohort suggests a potential resistance phenotype or aggressive tumor biology that does not respond to AFP decline, underscoring the need for alternative therapeutic strategies or combination regimens in this subgroup. This insight advocates for biomarker-informed clinical trials tailored to trajectory-defined patient subsets.
In the evolving landscape of hepatocellular carcinoma management, where immunotherapies and novel targeted agents are emerging, the integration of AFP trajectory monitoring could prove invaluable for treatment sequencing and personalized care. As therapeutic options diversify, robust biomarkers enabling early detection of resistance or response will become critical to optimize outcomes and resource allocation.
Moreover, these findings resonate amid global increases in liver cancer incidence associated with metabolic syndrome, viral hepatitis, and cirrhosis, particularly in regions with limited access to advanced imaging or biopsy capabilities. Serum biomarkers such as AFP, when leveraged with trajectory analysis, could democratize prognosis estimation and prompt timely therapeutic interventions across diverse healthcare settings.
The study by Zheng et al. thus provides a paradigm-shifting framework, transitioning AFP from a static diagnostic marker to a dynamic predictive tool capable of guiding individualized therapy in unresectable hepatocellular carcinoma. This advancement aligns with precision oncology’s goals: tailoring treatments based on patient-specific tumor biology, optimizing clinical outcomes, and minimizing unnecessary toxicity.
In sum, the identification of four distinct AFP trajectories with divergent survival outcomes under lenvatinib therapy heralds a new chapter in liver cancer management. By harnessing longitudinal biomarker data through advanced modeling techniques, oncology is poised to enhance prognostication and personalize systemic therapy in uHCC, transforming a grim prognosis into a more manageable condition.
Future prospective studies and clinical trials integrating AFP trajectory monitoring with molecular and imaging biomarkers could further refine and validate this approach. Ultimately, such multidisciplinary biomarker strategies will catalyze the evolution of hepatocellular carcinoma into a precisely targeted and adaptable clinical challenge, improving survival and quality of life for patients worldwide.
Subject of Research: Alpha-fetoprotein trajectories as predictive biomarkers in unresectable hepatocellular carcinoma patients receiving lenvatinib treatment.
Article Title: Trajectories of α-fetoprotein and unresectable hepatocellular carcinoma outcomes receiving lenvatinib: a retrospective, multicenter cohort study
Article References: Zheng, Y., Hu, J., Mei, Y. et al. Trajectories of α-fetoprotein and unresectable hepatocellular carcinoma outcomes receiving lenvatinib: a retrospective, multicenter cohort study. BMC Cancer 25, 1137 (2025). https://doi.org/10.1186/s12885-025-14516-y
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14516-y
Tags: advanced HCC managementalpha-fetoprotein dynamics in treatmentlenvatinib effectiveness in hepatocellular carcinomaliver cancer prognosislongitudinal data analysis in cancer researchmulticenter cohort study on liver cancerpatient outcome prediction in liver cancerprecision oncology advancementsstatistical modeling in oncologytherapeutic strategies for liver cancertreatment response monitoring in hepatocellular carcinomaunresectable hepatocellular carcinoma biomarkers