The unique intersection in the brain between the stress system and binge drinking may be the key to controlling the urge to binge drink, report Medical University of South Carolina researchers
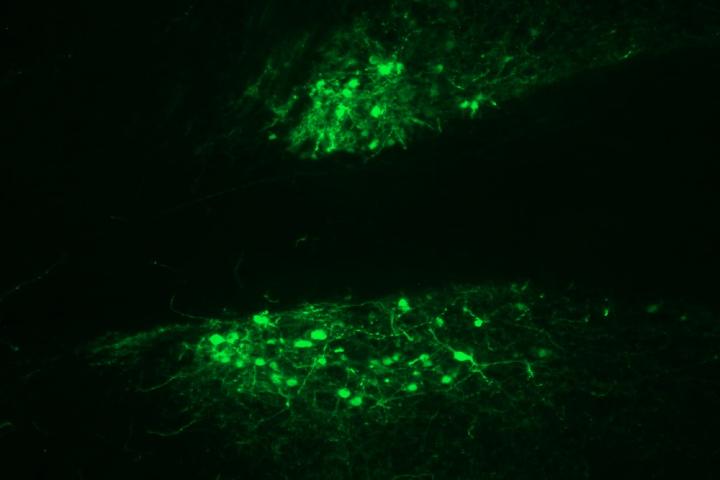
Credit: JR Haun, Medical University of South Carolina
A team of National Institutes of Health-funded researchers at the Medical University of South Carolina has found that deactivating a stress-signaling system in a brain area known for motivation and emotion-related behaviors decreases binge drinking. The study, which was published online in February and is to appear in the May issue of Neuropharmacology, pinpoints a particular system in a specific brain region that can be manipulated to reduce harmful binge drinking.
The MUSC team was led by Howard C. Becker, Ph.D., director of the Charleston Alcohol Research Center and professor in the Department of Psychiatry & Behavioral Sciences.
“Binge drinking is one of the most common patterns in which alcohol is consumed,” explained Becker. “It’s a risky behavior, and one consequence of repeated binge drinking is increasing risk for developing an alcohol use disorder.”
Further, according to Becker, those who consistently binge drink, particularly during adolescent and college years, have almost 10 times the risk of developing an alcohol use disorder.
But how much alcohol must be consumed to qualify a drinking session as a binge?
A binge, as defined by the National Institute on Alcohol Abuse and Alcoholism, or NIAAA, means drinking to the legal limit of intoxication within two hours. Becker put this into perspective.
“This is four standard drinks for a woman or five drinks for a male – consumed over about a two-hour period,” he explained.
JR Haun, a graduate student in the Becker laboratory and first author on the article, described what the NIAAA considers ‘standard’ related to certain beverage types.
“A drink is defined as roughly one 12-ounce can of beer, a five-ounce glass of wine or a standard 1.5 ounce shot of distilled spirits,” he explained, adding that the serving sizes can vary based on the percentage of pure alcohol in the drink.
In their study, Becker and Haun tested a potential strategy for reducing risky binge drinking.
“Binge drinking is a destructive behavior,” said Haun. “And our goal was to curb that. Through our investigation, we found a brain region and a system that we can manipulate to decrease binge drinking.”
The system that Becker’s team investigated – the opioid receptor system – is well-recognized in the addiction field.
Notorious narcotic drugs of abuse, such as morphine, heroin and oxycontin/oxycodone act on the opioid-receptor system, producing the pleasurable effects that make these drugs so addictive.
However, there is an odd opioid receptor out, so to speak, that is not involved in signaling pleasure.
“The kappa opioid-receptor system is the antithesis to other opioid receptors,” explained Haun. “It’s often referred to as an anti-reward system.”
Instead of feelings of pleasure, the kappa opioid receptor produces stress and discontent.
When people drink and experience positive effects, that is partially due to pleasurable opioid receptors being activated. However, after they have finished drinking and nausea, headache, and the stress of withdrawal start to set in, the kappa opioid receptor system has been activated.
Becker’s team found that turning off the kappa opioid receptors in the brain decreased binge drinking. This finding suggests that the kappa opioid receptor system is important not only in the negative state of withdrawal but also in driving binge drinking itself.
At first glance, this finding might sound counterintuitive. How does turning off the negative effects of the kappa opioid receptor decrease drinking?
“It’s not entirely clear why,” said Haun. “But what we do know is that kappa opioid receptors play an important role in the negative emotional state that drives drinking when it becomes compulsive in alcohol use disorders.”
Becker and Haun hypothesize that the kappa opioid receptor system may drive binge and compulsive alcohol use in a similar way, in addition to contributing to stress and unease during withdrawal.
To begin testing their hypothesis, Becker and Haun first identified the exact region in the brain that is involved in binge drinking driven by kappa opioid receptors.
Becker’s team homed in on a network of structures called the extended amygdala. According to Haun, it is a part of the brain that’s involved in motivational behavior, is very responsive to stress, and is implicated in compulsive drinking. This network of circuits in the brain also contains a number of kappa opioid receptors, making it the team’s top candidate to investigate for its role in regulating excessive drinking.
To determine how kappa opioid receptors in the extended amygdala affect binge drinking, Becker’s team specifically inactivated kappa opioid receptors in this region in mice.
“Haun actually introduced a drug that blocks kappa opioid receptors right into the extended amygdala,” explained Becker.
This study used a binge-drinking mouse model, which allowed the mice to drink freely for four hours each night.
“The mice will drink enough alcohol in this relatively short period of time to achieve blood alcohol levels that would define it as a binge episode,” said Becker.
After blocking the kappa opioid receptors in these mice, the team tested how much alcohol the animals voluntarily consumed. What they found could have important implications for future treatments of chronic binge drinking, according to Haun.
“Blocking these kappa receptors in the extended amygdala didn’t completely abolish drinking,” explained Haun. “It brought it down to a more moderate level, the equivalent being a glass of wine at dinner opposed to a bottle.”
This finding supports Becker and Haun’s hypothesis that the kappa opioid receptor system in the extended amygdala promotes binge drinking.
Blocking kappa opioid receptors in the extended amygdala, therefore, could act as a therapy to taper binge drinking.
So will there soon be a pill to curb the urge to binge?
According to Becker, if such a therapy were developed, he believes it would be best tailored for those who have difficulty controlling more chronic heavy drinking, such as those with an alcohol use disorder.
“I think the ultimate goal is to better understand new potential treatment targets and how new therapeutics may have some value in helping to quell the desire and motivation to drink excessively in those who have developed an alcohol use disorder or are on the threshold of doing so,” explained Becker.
###
Disclosure: The content of the article summarized here is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
About the Medical University of South Carolina
Founded in 1824 in Charleston, MUSC is the oldest medical school in the South as well as the state’s only integrated academic health sciences center with a unique charge to serve the state through education, research and patient care. Each year, MUSC educates and trains more than 3,000 students and 800 residents in six colleges: Dental Medicine, Graduate Studies, Health Professions, Medicine, Nursing and Pharmacy. The state’s leader in obtaining biomedical research funds, in fiscal year 2019, MUSC set a new high, bringing in more than $284 million. For information on academic programs, visit http://musc.
As the clinical health system of the Medical University of South Carolina, MUSC Health is dedicated to delivering the highest quality patient care available while training generations of competent, compassionate health care providers to serve the people of South Carolina and beyond. Comprising some 1,600 beds, more than 100 outreach sites, the MUSC College of Medicine, the physicians’ practice plan and nearly 275 telehealth locations, MUSC Health owns and operates eight hospitals situated in Charleston, Chester, Florence, Lancaster and Marion counties. In 2019, for the fifth consecutive year, U.S. News & World Report named MUSC Health the No. 1 hospital in South Carolina. To learn more about clinical patient services, visit http://muschealth.
MUSC and its affiliates have collective annual budgets of $3.2 billion. The more than 17,000 MUSC team members include world-class faculty, physicians, specialty providers and scientists who deliver groundbreaking education, research, technology and patient care.
Media Contact
Heather Woolwine
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




