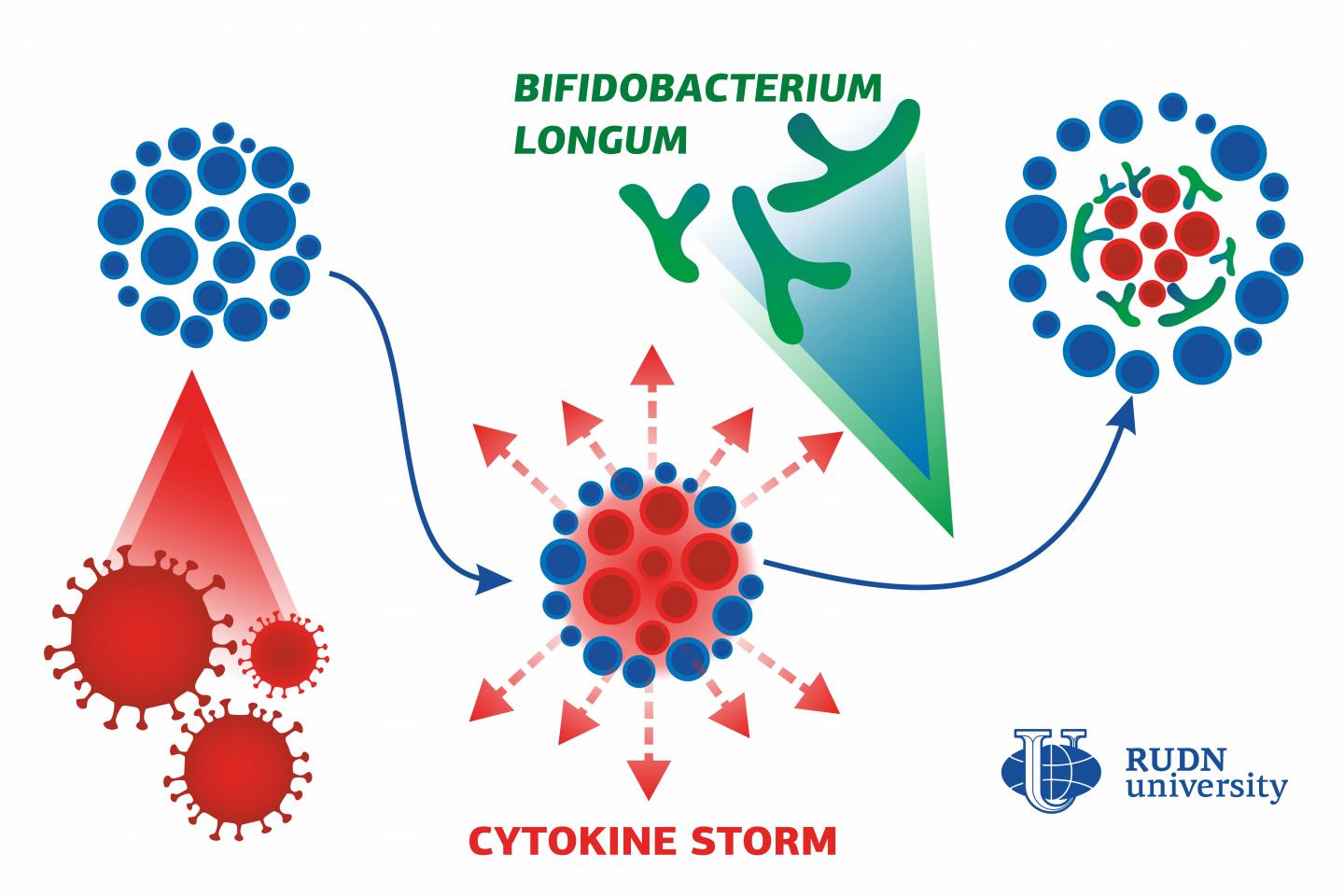
A geneticist from RUDN University studied the effect of Bifidobacterium (intestinal bacteria) on the inflammatory process and discovered that their surface protein is capable of stopping excessive or uncontrollable inflammation
Credit: RUDN Univeristy
A geneticist from RUDN University studied the effect of Bifidobacterium (intestinal bacteria) on the inflammatory process and discovered that their surface protein is capable of stopping excessive or uncontrollable inflammation, like the one observed in COVID-19 patients. A fragment of this protein can be used as an anti-inflammatory medication when treating coronavirus and other diseases. The results of the study were published in the Anaerobe journal.
When in danger, the cells of our body send out an SOS signal that is received by other cells and causes an immune response. This is how inflammation starts. This call to action is transmitted by special peptides known as anti-inflammatory cytokines. Sometimes there are too many of them, and a so-called cytokine storm occurs. This dangerous and sometimes deadly reaction is observed in severe cases of COVID-19. However, some pathogenic bacteria know how to trick our body’s protective systems: they use special proteins to capture cytokines and reduce inflammation. Until recently scientists had been unaware whether bifidobacteria–useful symbiotic microorganisms that live in our intestines–have the same effect on the inflammatory process. A geneticist from RUDN University was the first to demonstrate this mechanism.
The researchers conducted an experiment to study how FN3, a surface protein of Bifidobacterium longum, blocks or binds cytokines. FN3 helps cells attach to different surfaces, including intestinal walls covered in mucus. Moreover, it has two protein-carbohydrate moieties (fibronectin domains) that are similar to human cytokine receptors. The experiment showed that FN3 is able to bind TNF-α, one of the main cytokine storm factors.
To find out what specific cytokines are bound by FN3, the team used a method called ELISA (Enzyme-Linked ImmunoSorbent Assay) and applied it to a protein fragment with a fibronectin domain. First, antibodies that react only with FN3 were secured on a base. Then, a fragment of FN3, cytokines, and antibodies to them bound with a fluorescent tag were added. As a result, the team built a sandwich-like structure: antibody-FN3-cytokine-antibody.
Of four cytokines that belonged to different classes, only the tumor necrosis factor TNF-α showed effective binding. The fact that bifidobacterial surface proteins were able to recognize specific classes of cytokines supported the team’s theory: these bacteria are also capable of regulating our immune response.
Studies like this are especially important for understanding the processes of immune development in newborn babies, as their intestinal microbiome almost entirely consists of bifidobacteria. Biologists also believe that the tumor necrosis factor-specific fragment of FN3 can reduce the levels of cytokine storm in COVID-19 patients.
“Studies of cytokine-binding properties of microorganisms have become extremely important recently in view of the current epidemiological situation. Uncontrollable inflammation or cytokine storm is one of the most prominent elements of COVID-19 pathogenesis. Selective binding of TNF-α, one of the key factors of inflammation, with a fragment of the FN3 protein of Bifidobacterium longum opens a prospect for developing new medicinal drugs that would slow down the cytokine reaction. It has already been agreed that a preclinical trial of a new FN3-based anti-inflammatory medication should be conducted as quickly as possible,” said Prof. Valery Danilenko, a PhD in Biology from RUDN University.
###
The participants of the study also represented Mechnikov Research Institute of Vaccines and Sera and Vavilov Institute of General Genetics of the Russian Academy of Sciences.
Media Contact
Valeriya Antonova
[email protected]
Related Journal Article
http://dx.