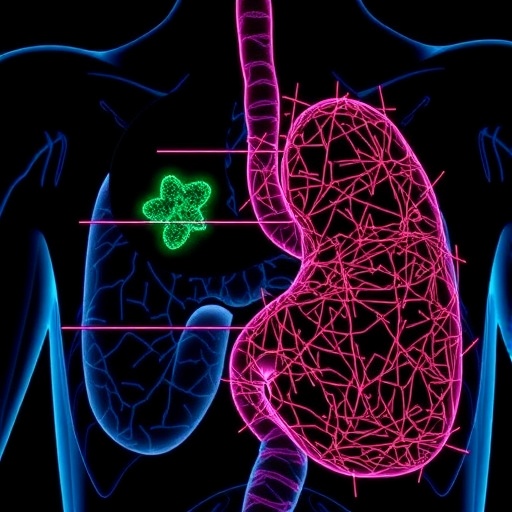
Tumor microenvironments (TMEs) are recognized as critical players in the progression of various types of cancers, including gastric cancer. Recent research by prominent scientists Lu, Zhang, Han, and colleagues has brought significant insights into how the complex interactions within the TME not only influence gastric cancer pathogenesis but also affect the tumor’s response to therapies. Understanding the dynamics of the TME allows for the identification of potential therapeutic targets, showcasing the need for comprehensive investigations into cellular behaviors within these environments.
The study provides a meticulous analysis of the components constituting the TME in gastric cancer, emphasizing the intricate relationship between cancer cells, immune cells, stromal cells, and the extracellular matrix. These components collaborate to create a unique microenvironment that not only supports tumor growth and survival but also orchestrates the tumor’s ability to resist conventional therapies. The interplay between tumor cells and their microenvironment thus becomes a focal point for developing novel therapeutic strategies aimed at overcoming this resistance.
A significant aspect of the research is its focus on the heterogeneity of the TME. Tumors are not monolithic; they consist of a diverse array of cell types, including cancer-associated fibroblasts, immune cells, and endothelial cells, each contributing to the TME’s overall behavior. This heterogeneity complicates treatment regimens because different cell populations may respond variably to therapeutic interventions, thereby necessitating a more nuanced approach to cancer therapy. It is crucial to consider this variability when devising treatment plans to enhance efficacy and minimize resistance.
Moreover, the study delves into the role of the immune system within the TME of gastric cancer. The presence and type of immune cells, such as tumor-infiltrating lymphocytes, can significantly influence the tumor’s growth and response to therapy. The researchers highlight that understanding the immune landscape is essential for predicting treatment outcomes and formulating personalized immunotherapies. By profiling the immune cell populations within gastric tumors, it’s possible to identify which patients may benefit from immunotherapy and which may not.
An additional layer of complexity arises from the stressors that tumors encounter, leading to adaptive changes within the TME. These stressors can involve nutrient deprivation, hypoxia, and elevated levels of reactive oxygen species. The researchers explore how these environmental challenges can drive tumor cells to undergo metabolic reprogramming and phenotypic changes that promote survival and proliferation. Recognizing these adaptive responses provides a foundation for targeting the metabolic pathways that support tumor resilience.
Furthermore, the findings underscore the significance of the extracellular matrix (ECM) in shaping the TME. The ECM serves not only as a structural scaffold but also as a dynamic entity that communicates with tumor cells through biochemical signals. Changes in ECM composition and stiffness can directly impact cell behavior, influencing migration, invasion, and resistance to therapy. By elucidating these interactions, the researchers propose the idea of targeting the ECM as a strategy to modify the TME and improve therapeutic outcomes.
Another notable aspect of this research is its exploration of the potential biomarkers related to the TME. Tumor microenvironmental factors can serve as indicators for both prognosis and response to treatment, guiding clinicians in making informed decisions. Identifying such biomarkers could lead to the development of predictive models that help in anticipating how a patient’s tumor will respond to specific therapies, leading to more tailored and effective treatment strategies.
The implications of these insights extend into the realm of combination therapies. By identifying specific features of the TME that contribute to therapeutic resistance, the researchers propose that a combination of immunotherapies and conventional treatments could yield better results. This layered approach could potentially overwhelm tumor defenses and improve patient outcomes by targeting multiple aspects of tumor biology simultaneously.
Additionally, the researchers emphasize the importance of early intervention. Understanding the early dynamics of the TME could allow for preventive strategies that inhibit tumor initiation and progression. By studying the initial interactions between normal cells and the potential tumor cells, it may be possible to identify key interventions that could halt cancer development before it progresses to advanced stages.
It is also noteworthy that the research advocates for a shift in focus from traditional tumor-centric models to a more holistic understanding of cancer biology. Rather than isolating tumor cells for study, considering the surrounding microenvironment is crucial for comprehensively addressing the challenges posed by gastric cancer. This paradigm shift could inspire innovative research methodologies and therapeutic strategies that reflect the multifaceted nature of cancer.
Lastly, the authors call for interdisciplinary collaboration between oncology, immunology, and molecular biology to foster innovations in treatment modalities. Through shared insights and advancements, the scientific community will be better equipped to tackle the complexities of the TME and its role in gastric cancer. Such collaborations could lead to breakthroughs that not only change the trajectory of gastric cancer treatment but also influence cancer therapies broadly.
The insights generated from this research on tumor microenvironment dynamics herald a new chapter in our understanding of gastric cancer. As researchers continue to unravel the complexities of the TME, the hope is to translate these findings into clinical applications that will ultimately improve the prognosis for patients battling this challenging disease.
Expanding our knowledge on how the TME influences cancer resilience and therapy response can lead to revolutionary changes in treatment paradigms. The future of gastric cancer management may very well hinge on our ability to modify the tumor microenvironment effectively, paving the way for more effective and personalized approaches to combatting this formidable disease.
In conclusion, the work of Lu, Zhang, Han, and their team is vital in illuminating the pathogenesis of gastric cancer and its resistance to treatments. By further exploring and integrating the dynamics of the TME into therapeutic planning, there exists an opportunity to dramatically improve patient outcomes and redefine expectations in cancer care.
Subject of Research: Tumor Microenvironment in Gastric Cancer Pathogenesis and Therapeutic Resistance
Article Title: Tumor microenvironment dynamics in gastric cancer pathogenesis and therapeutic resistance
Article References:
Lu, Z., Zhang, Q., Han, J. et al. Tumor microenvironment dynamics in gastric cancer pathogenesis and therapeutic resistance.
Mol Cancer (2026). https://doi.org/10.1186/s12943-026-02572-2
Image Credits: AI Generated
DOI: 10.1186/s12943-026-02572-2
Keywords: Gastric cancer, tumor microenvironment, therapeutic resistance, immunology, extracellular matrix, biomarkers, combination therapies, metabolic reprogramming.
Tags: cancer-associated fibroblasts in TMEcellular behaviors in tumor microenvironmentsextracellular matrix role in cancer progressionheterogeneity of tumor microenvironmentimmune response in gastric cancerinteractions within tumor microenvironmentsnovel therapeutic strategies for gastric cancerovercoming therapy resistance in gastric cancerresistance mechanisms in gastric cancerstromal cell contributions to TMEtherapeutic targets in gastric cancertumor microenvironment in gastric cancer