In an intriguing development within the field of neuroscience and gut health, recent research indicates that fecal microbiota transplantation (FMT) can significantly enhance neurogenesis in the hippocampus, particularly through the modulation of the Wnt signaling pathway. This groundbreaking study, led by Su et al., delves into the effects of FMT in a rat model suffering from chronic cerebral hypoperfusion, a condition often resulting in cognitive decline and neurodegeneration. The findings shed new light on the potential therapeutic applications of gut microbiota in treating neurological disorders.
The study investigates the complex interplay between gut health and brain function, underscoring the relevance of the gut-brain axis. This vital communication network between the gastrointestinal system and the central nervous system has garnered increasing attention in recent years, as emerging evidence suggests that gut flora can influence neural processes. Su et al. propose that restoring a healthy microbiome through FMT could mitigate the adverse effects of chronic cerebral hypoperfusion, a condition characterized by reduced blood flow to the brain.
Chronic cerebral hypoperfusion leads to a variety of neurological deficits, including memory impairment and decreased neurogenesis. The hippocampus, a key brain region associated with learning and memory, is particularly vulnerable to changes in cerebral blood flow. The researchers aimed to assess whether FMT could activate the Wnt signaling pathway, which is crucial for neurodevelopment and synaptic plasticity, thereby promoting neurogenesis in the hippocampus of rats subjected to chronic cerebral hypoperfusion.
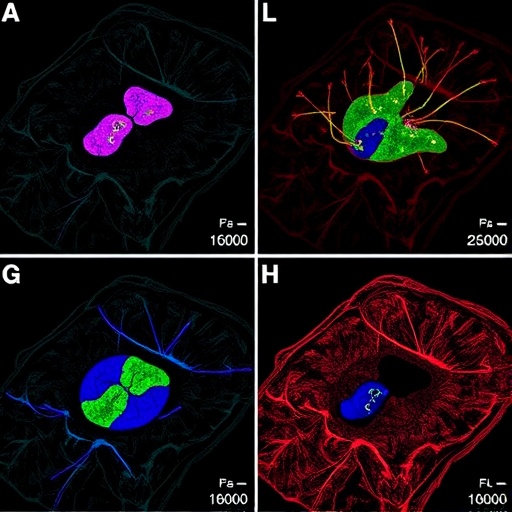
To achieve this, the authors conducted a series of well-designed experiments, where they first established a model of chronic cerebral hypoperfusion in rats. Following this, they performed fecal microbiota transplants from healthy donor rats to the hypoperfused rats. Their assessments involved detailed analysis of hippocampal neuron proliferation and differentiation, employing sophisticated techniques such as immunohistochemistry and RNA sequencing.
The results were striking. After undergoing FMT, the rats not only exhibited a marked increase in the proliferation of neural progenitor cells in the hippocampus but also demonstrated enhanced synaptic integrity. These findings suggest that the beneficial alterations in gut microbiota following transplantation could stimulate the activation of the Wnt3a pathway, a key player in promoting cellular growth and differentiation within the brain.
One of the most remarkable aspects of this research is the identification of specific microbial species that appeared to drive these neurogenic effects. The study highlighted the selective enrichment of certain beneficial bacteria post-transplant, suggesting that a diverse and balanced gut microbiome is essential for optimal brain health. The authors speculate that these microbes may secrete metabolites capable of influencing brain function, thereby bridging the gap between gut health and neurogenesis.
Additionally, the study contributes to an evolving narrative about the potential of non-invasive therapies in neurological conditions. While traditional pharmacological approaches often focus on symptom management, this research points toward innovative methods that target the root causes of cognitive decline. By harnessing the power of gut microbiota, FMT could pave the way for novel treatments in patients suffering from neurodegenerative conditions or cognitive impairments linked to vascular health.
The implications of these findings extend beyond animal models, sparking curiosity about the potential for similar therapeutic effects in humans. While clinical trials are essential for validating these results in human populations, the promise of utilizing gut microbiota to enhance cognitive function is an exciting frontier in neuroscience. The prospect of developing microbiota-based therapies could revolutionize how doctors approach neurodegenerative diseases.
Moreover, this study raises important questions about diet, lifestyle, and their effects on gut health and, consequently, brain health. As research continues to elucidate the connections between the microbiome and neural processes, it becomes increasingly clear that a holistic approach to health is vital. Personalized nutrition and microbiome management could become key strategies in promoting not only gut health but also cognitive resilience.
Furthermore, the findings emphasize the need for greater public awareness regarding the complexities of gut microbiota and its far-reaching implications for mental health and cognitive function. As the stigma surrounding mental health continues to diminish, educating individuals about the role of their gut health in overall well-being is paramount. It encourages a proactive approach to maintaining a balanced lifestyle that includes a diverse diet rich in prebiotics and probiotics.
The story does not end here. Ongoing research will undoubtedly delve deeper into the molecular mechanisms behind these observations, exploring the potential of targeting specific microbial communities to facilitate neurogenesis. Future studies may uncover additional pathways influenced by gut microbiota, further unraveling the intricate connections between our gut and brain.
The research led by Su et al. stands as a testament to the importance of interdisciplinary collaboration in science. Bridging the fields of microbiology, neuroscience, and nutrition, this study exemplifies how innovative thinking can yield transformative insights into complex biological systems. It serves as a reminder of the extensive potential that lies in understanding and harnessing the microbiome for health benefits.
As we move forward into an era where personalized medicine becomes increasingly viable, findings like these will play a crucial role in shaping future therapeutic protocols. With the promise of fecal microbiota transplantation gaining traction, clinicians may soon find themselves equipped with novel tools to address cognitive decline among patients and advocate for preventive strategies aimed at preserving brain health.
In conclusion, the pioneering work of Su et al. highlights a hopeful future where understanding the gut microbiome could lead to groundbreaking interventions for cognitive impairment and neurodegenerative diseases. As scientists unravel the complexities of the gut-brain axis, the potential to transform patient care and improve quality of life becomes increasingly tangible.
In summary, the research demonstrates that fecal microbiota transplantation not only improves gut health but may also lead to significant advancements in neurogenesis and cognitive function. This multifaceted relationship showcases the untapped therapeutic potential of leveraging gut microbiota for neurological benefits. Researchers and healthcare professionals alike should continue to explore this exciting domain, ensuring that future generations benefit from enhanced understanding and innovative solutions for brain health.
Subject of Research: Fecal microbiota transplantation and its effects on hippocampal neurogenesis in chronic cerebral hypoperfusion.
Article Title: Fecal microbiota transplantation promotes Wnt3a-mediated hippocampal neurogenesis in a rat model of chronic cerebral hypoperfusion.
Article References:
Su, SH., Lu, DD., Wu, YF. et al. Fecal microbiota transplantation promotes Wnt3a-mediated hippocampal neurogenesis in a rat model of chronic cerebral hypoperfusion. J Transl Med (2026). https://doi.org/10.1186/s12967-025-07631-8
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07631-8
Keywords: fecal microbiota transplantation, neurogenesis, Wnt3a, hippocampus, chronic cerebral hypoperfusion, gut-brain axis, cognitive decline, microbiome, neuroscience.
Tags: chronic brain blood flow issueschronic cerebral hypoperfusioncognitive decline treatmentfecal microbiota transplantationgut health and brain functiongut-brain axis communicationhippocampus neuroprotectionmicrobiome restoration benefitsneurogenesis enhancementneurological disorders therapyresearch in neuroscience and gut healthWNT signaling pathway modulation