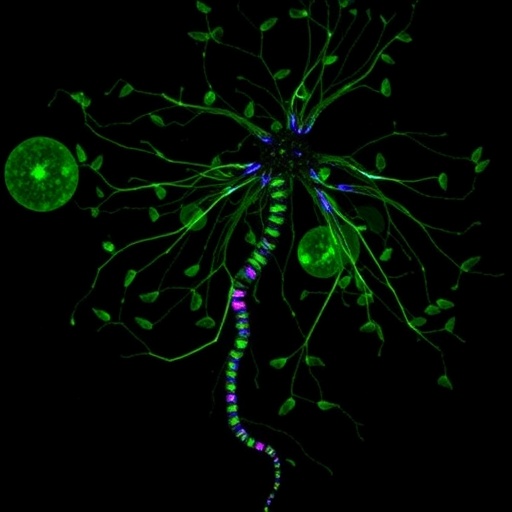
In a groundbreaking discovery that promises to illuminate the complex interplay between the immune system and neuronal health, researchers have unveiled a mechanism by which microglial CX3CR1 deficiency regulates the vulnerability of cone photoreceptors within the mouse retina. This finding heralds new avenues for understanding retinal diseases and potentially developing targeted therapies for conditions that lead to photoreceptor degeneration, thereby preserving vision.
Microglia, the resident immune cells of the central nervous system, have long been known to maintain the delicate balance of homeostasis in the neural environment. They are not just passive defenders that respond to injury; they actively modulate neuronal health and the response to degeneration. The study led by Li, Zhang, and Wang (2026) delves into the signaling pathways activated when the CX3CR1 receptor—a crucial communications hub for microglial cells—is deficient. This receptor is pivotal for microglia’s ability to interact with surrounding neurons, particularly under stress or pathological conditions.
In the mouse retina, cone photoreceptors are crucial for high-acuity vision and color perception. The loss or dysfunction of these cells can have dire consequences, including visual impairment or complete blindness. The research outlined how a deficiency in CX3CR1 expression leads to an altered microglial response, which ultimately translates into an increased susceptibility of cone photoreceptors to various stressors. This relationship between microglial signaling and photoreceptor vulnerability emphasizes the importance of immune signaling in retinal health.
One of the key pathways identified in this study involves the activation of STAT3, a transcription factor known for its role in mediating cellular responses to various stimuli. When microglial CX3CR1 is absent, STAT3 becomes aberrantly activated, which seems to trigger the release of cytokines and other signaling molecules that, rather paradoxically, exacerbate oxidative stress in cone photoreceptors. This amplification of stress signaling could explain why certain photoreceptors are selectively vulnerable in states of microglial dysregulation, offering insights into the immune and inflammatory factors contributing to retinal degeneration.
Moreover, the researchers explored the role of chemokines in this mechanism, specifically CCL and its interaction with ACKR1, a receptor that modulates chemokine signaling. The interplay between these molecules is crucial in shaping the local microenvironment of the retina, further influencing photoreceptor health. The dysregulation of these signaling pathways, as highlighted by the study, underlines the importance of tightly controlled microglial activity for the maintenance of retinal integrity.
The implications of this research extend beyond just understanding cone photoreceptor vulnerability. By dissecting the roles that microglial signaling pathways play in retinal health, the study raises the possibility of developing targeted therapeutic interventions aimed at modulating immune responses to protect vision. For instance, therapies aimed at ameliorating CX3CR1 deficiencies or modulating STAT3 activity could offer promising strategies for preserving cone photoreceptors in individuals at risk for retinal degeneration.
The impact of microglial signaling on retinal disorders could also reshape how we approach aging-related macular degeneration and other forms of retinal disease. As the population ages, the incidence of these diseases is expected to rise, emphasizing the need for innovative solutions. Understanding the molecular underpinnings discussed in Li, Zhang, and Wang’s research provides a vital framework for future investigations aimed at harnessing the immune system for neuroprotective strategies.
Furthermore, the link between microglial dysfunction and cone photoreceptor vulnerability opens an exciting dialogue about the role of immune dysregulation in a wider array of neurological diseases. As researchers continue to decode the complexities of microglial interactions with neural cells, we may uncover parallels in other regions of the central nervous system, thereby unearthing multisystem therapeutic opportunities.
It’s important to note that while the findings are promising, translating these laboratory insights into clinical interventions will require extensive research. This includes validating the mechanisms uncovered in human retinal tissues and exploring the multifaceted roles that microglia play in various retinal pathologies. The quest to bridge the gap between basic research and clinical application remains a formidable, yet necessary, endeavor.
As the scientific community digests these findings, collaborative efforts will be paramount. Researchers from disciplines spanning immunology, neurology, and ophthalmology will need to join forces to advance our understanding of microglial functions within the retina. Such interdisciplinary efforts could yield innovative strategies to combat retinal diseases and improve the quality of life for those affected.
The study by Li and colleagues is part of a growing body of literature that emphasizes the importance of the immune system in neuronal health. As we continue to unravel the complexities of microglial signaling, it becomes ever more clear that these cells are not merely defenders against disease but are integral to maintaining the neural ecosystem. Their findings call for a reevaluation of therapeutic approaches that consider the immune system’s role in protecting neurons.
This research is not merely an academic exercise; it carries profound ramifications for public health. As millions face the threat of vision loss due to retinal diseases, understanding the underlying mechanisms of cone photoreceptor vulnerability could lead to transformative interventions. By leveraging insights from the immune response and its influence on neuronal health, we inch closer to safeguarding vision for future generations.
In conclusion, as we reflect on the journey ahead, the study by Li, Zhang, and Wang serves as a beacon illuminating the path forward in retinal research. The intersection of immunology and neuroscience is a fertile ground for discovery, making it an exciting time for scientists and clinicians alike. The quest to harness the power of the immune system to protect our most precious sense, vision, is a challenge that science is ready to tackle.
Subject of Research: Microglial CX3CR1 deficiency and its impact on cone photoreceptor vulnerability in the mouse retina.
Article Title: Microglial CX3CR1 deficiency regulates the selective vulnerability of cone photoreceptors via STAT3/CCL–ACKR1 signaling in the mouse retina.
Article References:
Li, R., Zhang, J., Wang, Q. et al. Microglial CX3CR1 deficiency regulates the selective vulnerability of cone photoreceptors via STAT3/CCL–ACKR1 signaling in the mouse retina.
Exp Mol Med (2026). https://doi.org/10.1038/s12276-025-01618-7
Image Credits: AI Generated
DOI: 15 January 2026
Keywords: Microglia, CX3CR1, cone photoreceptors, retinal degeneration, STAT3, CCL, ACKR1, vision, immune system.
Tags: cone photoreceptor vulnerabilityhigh-acuity vision and color perceptionimmune modulation in the retinamicroglial CX3CR1 deficiencymicroglial-neuronal interactions.mouse retina studiesneuronal health and immune systemphotoreceptor degeneration mechanismsretinal diseases researchsignaling pathways in microgliatargeted therapies for vision preservationvisual impairment causes