In the dynamic realm of reproductive medicine, the intricate web of hormonal interactions plays a pivotal role in determining the success of assisted reproductive technologies, particularly in conditions like polycystic ovarian syndrome (PCOS). A recent groundbreaking study conducted by a team led by researchers Peng, H., Wang, L., and Jiang, J. illuminates the impact of elevated basal luteinizing hormone (LH) levels on in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) outcomes in patients diagnosed with PCOS. This retrospective analysis provides critical insights that could influence clinical decisions and patient management strategies in reproductive health.
PCOS is a prevalent endocrine disorder affecting women of reproductive age, characterized by a range of symptoms including irregular menstrual cycles, hyperandrogenism, and ovarian dysfunction. The complications associated with this condition often extend beyond fertility challenges, influencing metabolic health and psychological well-being. Given the complexity of PCOS, understanding how hormonal levels interact during fertility treatments is essential for optimizing patient outcomes.
At the heart of this investigation lies the hormone luteinizing hormone. LH, which is produced by the pituitary gland, plays a crucial role in regulating the menstrual cycle and ovulation. High basal levels of LH have long been hypothesized to correlate with adverse reproductive outcomes in women undergoing fertility treatments. The authors meticulously analyzed the data collected from a cohort of women with PCOS who underwent IVF or ICSI, aiming to ascertain the specific effects of elevated LH levels on their treatment success.
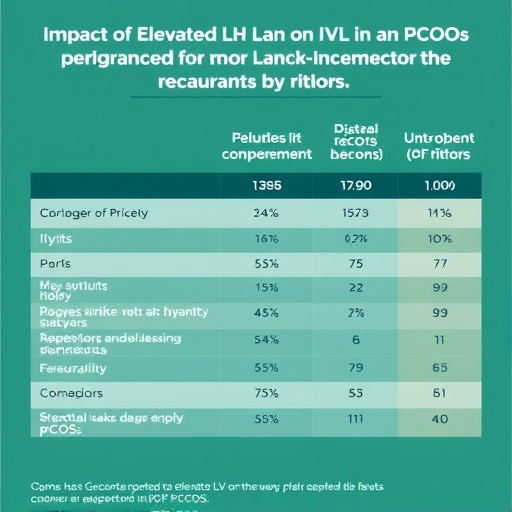
The study meticulously examined a diverse patient population, considering factors such as age, body mass index (BMI), and ovarian reserve markers. These variables are paramount in assessing the outcomes of fertility treatments, as they influence the overall responsiveness of the ovaries to stimulation protocols. By stratifying patients based on their basal LH levels, the researchers were able to uncover patterns that could elucidate the relationship between hormonal milieu and reproductive success.
Among the striking findings, the study revealed that high basal LH levels were associated with lower implantation and clinical pregnancy rates. This observation underscores the intricate balance required between LH and other hormones, particularly follicle-stimulating hormone (FSH), during the controlled ovarian stimulation process that is fundamental to IVF and ICSI procedures. The implications of these results suggest that clinicians may need to adjust treatment protocols for patients with high LH levels, potentially employing adjunct therapies to mitigate adverse effects.
Another compelling aspect of the study is the investigation of ovarian response during stimulation cycles. The results indicated that patients with elevated LH experienced altered ovarian follicle development, leading to an imbalance that could culminate in suboptimal egg quality. The quality of oocytes retrieved during these procedures is a significant determinant of the overall success rates in assisted reproductive technologies, as higher quality eggs are more likely to lead to viable embryos.
Although the findings of this research present a significant leap forward in understanding the hormonal dynamics in women with PCOS, they also highlight the complexities involved in personalizing treatment for different patient populations. The individual variability in hormonal responses necessitates a tailored approach in fertility management, particularly for patients with endocrine disorders like PCOS. This study reinforces the need for further research into the mechanistic pathways influenced by high LH levels and their implications for fertility.
As the scientific community continues to explore these associations, a broader dialogue surrounding the standardization of hormonal assessments prior to fertility treatments is emerging. Clinicians may soon have access to more refined protocols that facilitate better predictions of treatment outcomes based on hormonal profiles. This evolution in practice could optimize the allocation of resources and improve patient counseling regarding their chances of success during treatments.
The implications extend beyond mere statistics; they touch the lives of women and couples striving to overcome the challenges of infertility. Each percentage point in improved success rates represents a monumental shift in hope and potential for those affected by these conditions. As healthcare providers sift through the findings of this research, they are empowered to make informed decisions that reverberate through the experiences of their patients.
The study opens avenues for further investigations, probing additional hormones that might interact with or counterbalance the effects of LH. One intriguing area of exploration involves the interplay between LH and insulin—a hormone closely associated with metabolic syndrome in PCOS patients. Understanding how these two hormones interact could yield novel insights into improving fertility outcomes and managing PCOS as a multifaceted syndrome.
Moreover, the findings may stimulate interest in developing adjunct therapies targeting elevated LH levels. Treatments that can effectively modulate hormonal balance could become integral components of fertility protocols for women with PCOS, significantly enhancing their treatment experience and outcomes.
As researchers, clinicians, and patients absorb the implications of this study, it is clear that reproductive endocrinology is entering a new phase. One where the management of hormonal imbalances is becoming a standard consideration in fertility treatments, reflecting the evolving nature of evidence-based practices in reproductive health.
In conclusion, the research conducted by Peng and colleagues marks a significant advancement in the understanding of how elevated basal LH levels impact IVF and ICSI outcomes in women with PCOS. The study lays the groundwork for future investigations while emphasizing the importance of personalized care in reproductive medicine. With continued research and clinical application, there is hope for improving the landscape of fertility treatments for those affected by this challenging condition.
Subject of Research: High basal luteinizing hormone levels and their effects on IVF/ICSI outcomes in polycystic ovarian syndrome.
Article Title: Effects of high basal luteinizing hormone levels on in vitro fertilization/intra-cytoplasmic injection outcomes in polycystic ovarian syndrome: a retrospective study.
Article References:
Peng, H., Wang, L., Jiang, J. et al. Effects of high basal luteinizing hormone levels on in vitro fertilization/intra-cytoplasmic injection outcomes in polycystic ovarian syndrome: a retrospective study.
J Ovarian Res 18, 302 (2025). https://doi.org/10.1186/s13048-025-01899-6
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13048-025-01899-6
Keywords: Polycystic Ovarian Syndrome, Luteinizing Hormone, IVF, ICSI, Fertility Treatments.
Tags: assisted reproductive technology and PCOSelevated luteinizing hormone in PCOShormonal profiles and reproductive outcomeshormonal regulation in reproductive healthimpact of hormonal interactions on fertilityimplications of high LH on IVF successIVF outcomes in polycystic ovarian syndromeluteinizing hormone and in vitro fertilizationmanaging fertility in PCOS patientsreproductive medicine and PCOSretrospective analysis of LH levelsunderstanding PCOS and assisted reproduction