In a groundbreaking study poised to reshape the diagnostic landscape of prostate cancer, researchers have harnessed the power of habitat-based MRI radiomics to delve deep into the enigmatic realm of intratumoral heterogeneity. This innovative methodology addresses the critical challenge of identifying aggressive prostate cancer phenotypes, particularly those with high Gleason scores and a propensity to evolve into castration-resistant prostate cancer (CRPC), a formidable adversary in clinical oncology.
Prostate cancer’s clinical complexity stems largely from its heterogeneous nature, where varying cellular characteristics within a single tumor influence disease progression and treatment response. The Gleason score, a pivotal grading system, stratifies prostate cancer aggressiveness, with higher scores correlating with poor prognosis and resistance to conventional therapies. However, non-invasive, reliable preoperative assessments remain elusive, often leading to delayed interventions and suboptimal outcomes.
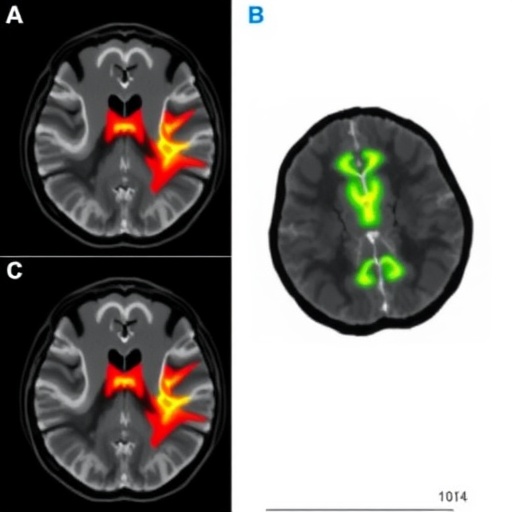
The research team embarked on a retrospective exploration, integrating conventional MRI modalities — T2-weighted imaging (T2WI), diffusion-weighted imaging (DWI), and apparent diffusion coefficient (ADC) maps — from a robust cohort of 264 patients diagnosed with prostate cancer. These diverse imaging techniques offer complementary insights, capturing structural, cellular, and microenvironmental tumor attributes, essential for comprehensive radiomic analysis.
Central to their approach was the concept of habitat imaging (HI), which partitions tumors into distinct microenvironmental subregions, or habitats, illuminating the spatial variation within the malignancy. This paradigm shift enables the quantification of intratumoral heterogeneity (ITH) via advanced radiomic features extracted from these habitats, transcending traditional whole-tumor analyses that often overlook subtle but clinically significant variations.
The study unfolded through two pivotal tasks. The first task aimed to discriminate between high and low Gleason scores using radiomic signatures derived from the entire tumor and habitat-specific heterogeneity metrics. Employing sophisticated multivariate logistic regression allowed the identification of independent clinical variables to be integrated with radiomic data, culminating in a composite predictive model. This integrative strategy not only enhanced predictive capabilities but also underscored the synergistic potential of combining imaging biomarkers with clinical parameters.
In this initial phase, the cohort was judiciously split into training and validation subsets, ensuring rigorous evaluation protocols. The intratumoral heterogeneity model outperformed traditional radiomics, achieving remarkable area under the curve (AUC) values of 0.892 in training and 0.826 in validation datasets. These metrics underscore the model’s robust discriminatory power, positioning it as a potential game-changer in preoperative risk stratification.
Building upon these insights, the second task concentrated exclusively on patients harboring high-Gleason score tumors, probing the capacity of habitat-based radiomic signatures to foresee the emergence of CRPC within a year following androgen deprivation therapy (ADT). Among 142 patients followed longitudinally, a subset developed CRPC, enabling the evaluation of predictive accuracy through receiver operating characteristic (ROC) curve and decision curve analyses.
Remarkably, the habitat-based heterogeneity model demonstrated superior prediction accuracy with AUC scores of 0.802 and 0.840 across training and testing sets, respectively. These findings highlight the potential of habitat radiomics as an early warning system for therapy resistance, thereby advocating for more personalized, timely interventional strategies.
Such strides in imaging informatics epitomize the broader scientific movement towards personalized oncology. By leveraging non-invasive imaging to capture tumor heterogeneity in vivo, clinicians can foresee aggressive disease courses and tailor therapies accordingly. This reduces the reliance on invasive biopsies and complements molecular diagnostics, deeply enriching the clinical decision-making arsenal.
Furthermore, the implications extend beyond prognostication. Habitat-based MRI radiomics could guide adaptive therapeutic planning, enabling oncologists to monitor intratumoral dynamics and anticipate evolving resistance patterns with unprecedented granularity. This could revolutionize the management of prostate cancer, shifting paradigms from reactive treatments to proactive, precision-based protocols.
Crucial to the study’s success was the meticulous integration of quantitative imaging features with sophisticated statistical modeling. The multivariate logistic regression ensured that the combined model capitalized on orthogonal information streams, capturing both morphological and microenvironmental nuances of tumor biology. This methodological rigor lends credence to the robustness and reproducibility of the findings.
Moreover, the extensive validation framework underscores the translational potential of this technology. By demonstrating consistent predictive performance across independent cohorts, the model positions itself as a viable candidate for clinical trials, and eventually integration into routine diagnostic workflows.
The study also shines a light on the urgent need for standardized radiomic protocols. Variability in MRI acquisition parameters and image preprocessing can significantly affect radiomic feature stability and, by extension, model accuracy. Addressing these technical challenges through harmonization efforts will be pivotal in realizing the full clinical potential of habitat-based radiomics.
Experts herald this study as a testament to the synergy between advanced imaging and computational analytics in unraveling cancer’s intricate heterogeneity. As the oncology community rallies around precision medicine, such pioneering approaches will be instrumental in decoding the complex tumor ecosystem, paving the way for breakthroughs in cancer prognosis and therapeutic management.
In conclusion, this retrospective analysis presents compelling evidence that habitat-based MRI radiomics, through quantification of intratumoral heterogeneity, offers an unparalleled window into the aggressiveness of prostate cancer and its resistance trajectory. As the field advances, these imaging biomarkers could transition from experimental tools to clinical mainstays, dramatically enhancing patient stratification, treatment planning, and ultimately, survival outcomes.
Subject of Research: Prostate cancer; intratumoral heterogeneity; habitat-based MRI radiomics; Gleason score prediction; castration-resistant prostate cancer prediction.
Article Title: Quantification of intratumoral heterogeneity using habitat-based MRI radiomics for predicting high-Gleason scores and castration-resistant PCa: retrospective study.
Article References:
Zhai, CF., Yang, X., Qi, X. et al. Quantification of intratumoral heterogeneity using habitat-based MRI radiomics for predicting high-Gleason scores and castration-resistant PCa: retrospective study. BMC Cancer (2025). https://doi.org/10.1186/s12885-025-15300-8
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-15300-8
Tags: aggressive prostate cancer predictioncastration-resistant prostate cancer identificationdiffusion-weighted imaging applicationsGleason score and prognosishabitat-based imaging in oncologyintratumoral heterogeneity analysismicroenvironmental tumor characteristicsMRI radiomics for prostate cancernon-invasive cancer assessment techniquesradiomic features in tumor analysisretrospective MRI study in prostate cancerT2-weighted imaging in cancer diagnosis