The relentless pursuit of innovative cancer therapies has reached a thrilling frontier with the emergence of metallic nanostructure-based photothermal therapy (PTT), a cutting-edge approach showing immense promise in the battle against metastatic tumors. In an in-depth review published in Medical Oncology, Begum and colleagues outline the transformative potential of exploiting metallic nanostructures to evoke precise, localized hyperthermia capable of destroying cancer cells while minimizing harm to surrounding tissue. This strategy stands poised to revolutionize how oncologists manage one of cancer’s deadliest attributes: its capacity to metastasize and colonize distant organs.
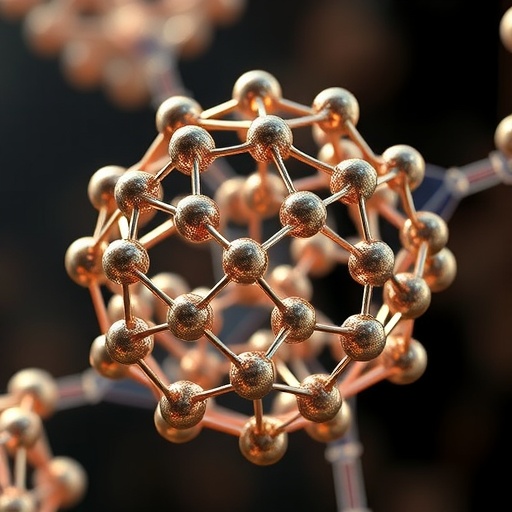
At the heart of this innovation lies the unique optical and thermal properties of metallic nanostructures, particularly gold and silver nanoparticles, which exhibit exceptional plasmonic resonance when exposed to near-infrared (NIR) light. This resonance enables efficient conversion of light energy into localized heat at the nanoscale, effectively generating hyperthermic conditions lethal to tumor cells. Unlike conventional thermal therapies, metallic nanostructure-based PTT offers unparalleled precision, as these engineered particles selectively accumulate in tumor microenvironments through enhanced permeability and retention (EPR) effects and targeted ligand modifications, thereby sparing healthy tissues.
Recent advances have significantly refined the design and functionalization of metallic nanostructures, optimizing their size, shape, and surface chemistry to enhance biocompatibility, tumor targeting, and photothermal conversion efficiency. Among the myriad configurations, gold nanorods, nanoshells, and nanostars have emerged as frontrunners, each offering distinctive advantages in tuning optical absorption to the NIR window—a spectral region where biological tissues exhibit maximum transparency. This spectral tuning is crucial for effective deep-tissue penetration, allowing the photothermal effect to reach tumors located beneath the skin’s surface, a key limitation in earlier PTT approaches.
Beyond the physical engineering, researchers are exploiting nanostructures as multifunctional platforms capable of integrating diagnostic and therapeutic modalities. These so-called theranostic agents combine photoacoustic imaging capabilities with photothermal effects, enabling real-time monitoring of nanoparticle distribution and therapeutic progress. Such dual-functionality not only improves treatment precision but also provides invaluable feedback for personalized cancer management, allowing clinicians to adapt intervention strategies dynamically.
One of the most exciting facets of metallic nanostructure-based PTT is its potential synergy with other treatment modalities, including chemotherapy, immunotherapy, and radiotherapy. By integrating metallic nanoparticles with chemotherapeutic drugs or immunostimulatory agents, researchers have demonstrated enhanced tumor regression and reduced systemic toxicity. Photothermal heating can disrupt tumor cell membranes and sensitize cancer cells to chemotherapeutic agents, while localized hyperthermia can also modulate the tumor microenvironment to facilitate immune cell infiltration, potentially overcoming immune evasion mechanisms inherent to metastatic cancers.
Despite these advances, translating metallic nanostructure-based PTT from bench to bedside poses several formidable challenges. Key concerns revolve around nanoparticle pharmacokinetics, biodistribution, and long-term safety profiles. The body’s mononuclear phagocyte system often sequesters nanoparticles in the liver and spleen, potentially leading to off-target accumulations and toxicity. Consequently, elaborate surface modifications, including polyethylene glycol (PEG) coating and biomimetic cloaking with cell membranes, are under intense investigation to extend circulation time and evade immune clearance.
Moreover, the heterogeneity of tumor microenvironments across different cancer types and metastatic sites complicates nanoparticle delivery and photothermal efficacy. Hypoxic and acidic tumor niches can alter nanoparticle accumulation and heat generation, necessitating tailored nanostructure designs and treatment protocols. Advanced modeling and machine learning techniques are being harnessed to predict treatment outcomes and optimize the parameters of PTT, from laser wavelength and intensity to nanoparticle dosage, ensuring maximal therapeutic benefit with minimal adverse effects.
The clinical landscape has started to witness the integration of metallic nanostructure-based photothermal therapy into early-phase trials, signaling a pivotal turning point. Initial results underscore the feasibility, safety, and potent anti-tumor effects of this approach in patients with advanced metastatic disease, sparking optimism for its incorporation into standard oncological practice. Importantly, the minimally invasive nature of PTT offers a welcome alternative for patients ineligible for surgery or systemic chemotherapy, enhancing quality of life alongside extending survival.
Beyond oncology, this versatile technology portends applications in antimicrobial therapies, targeted drug delivery, and even neural modulation, illustrating the broad impact of metallic nanostructures in biomedical science. The versatility of these engineered particles to generate controlled thermal effects upon NIR irradiation is opening new horizons in precision medicine, where thermal energy is harnessed as a tool for not just destruction but modulation of biological functions.
In parallel with experimental efforts, regulatory frameworks and manufacturing processes are evolving to ensure the scalable production of high-quality nanostructures with consistent properties, a prerequisite for widespread clinical adoption. Collaboration across multidisciplinary teams comprising chemists, engineers, biologists, and clinicians is accelerating, driving innovation and standardizing methodologies critical for robust and reproducible outcomes.
Public and private investment in nanomedicine research continues to surge, reflecting growing confidence in the transformative potential of metallic nanostructure-based photothermal therapy. Funding initiatives emphasize not only technological advancement but also addressing health disparities by developing cost-effective therapies accessible to diverse global populations afflicted by metastatic cancers.
The excitement surrounding this technology extends beyond academia and clinical circles, capturing the imagination of the wider public as a beacon of hope against the scourge of metastatic cancer. Social media and science communication platforms are amplifying awareness, fostering informed dialogues about the promises and challenges of nanoscale photothermal interventions, and highlighting the importance of rigorous science in translating lab discoveries into life-saving treatments.
In conclusion, metallic nanostructure-based photothermal therapy epitomizes the confluence of nanotechnology and oncology, offering a sophisticated weapon to outsmart cancer metastasis. Through exquisite control of light, heat, and nanoscale engineering, this emerging modality paves the way for therapies that are not only more effective but also less debilitating, marking a paradigm shift in cancer care. As the field matures, continued innovation, meticulous clinical validation, and ethical deployment will define the trajectory of this ground-breaking approach in transforming patient outcomes worldwide.
Subject of Research: Metallic nanostructure-based photothermal therapy for cancer metastasis management
Article Title: Recent advances in metallic nanostructure-based photothermal therapy in the management of cancer metastasis.
Article References:
Begum, R.F., Afreen, N., Nirenjen, S. et al. Recent advances in metallic nanostructure-based photothermal therapy in the management of cancer metastasis. Medical Oncology 42, 515 (2025). https://doi.org/10.1007/s12032-025-03075-8
Image Credits: AI Generated
Tags: advances in cancer metastasis managementbiocompatibility of metallic nanoparticlesengineered nanoparticles for tumor targetingenhanced permeability and retention effect in tumorsgold and silver nanoparticles in oncologylocalized hyperthermia for cancer treatmentMedical Oncology advancements in cancer researchmetallic nanostructures in cancer therapyphotothermal therapy for metastatic tumorsplasmonic resonance in nanomedicineprecision cancer therapiestargeted cancer treatment innovations