Giant omphaloceles present a unique challenge in neonatology, drawing attention to their complex management and the necessity for innovative treatment strategies. Recent advancements in surgical techniques and patient care approaches have led to a transformative perspective on how these congenital defects can be treated. Notably, a systematic review conducted by a group of researchers has presented compelling evidence for the efficacy of a waiting treatment model, providing a comprehensive outlook on the future for infants diagnosed with giant omphaloceles.
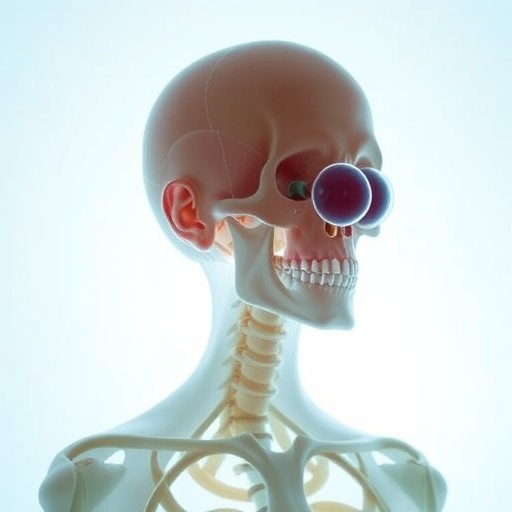
In essence, giant omphaloceles are characterized by a significant defect in the abdominal wall, allowing the intestines and, in some cases, other abdominal organs, to protrude through the skin. This condition not only poses immediate health risks but also raises concerns about potential long-term complications. The clinical decisions surrounding surgical intervention are critically important, and the timing of surgery often has profound implications for the infant’s development and overall well-being.
The investigating team, comprising Pan, Zhou, Li, and others, embarked on a detailed exploration of the varied approaches historically employed in managing giant omphaloceles. Their systematic review meticulously dissected existing literature to determine the optimal course of action—a task that necessitated a keen understanding of both the medical and psychological aspects surrounding this condition. By synthesizing data from numerous studies, the authors aimed to discern patterns and outcomes that could inform best practices and clinical guidelines.
One of the most significant findings of the review is the argument for a conservative waiting treatment model, wherein clinicians may opt to postpone surgical intervention in selected cases. This approach is predicated on the recognition that many infants with giant omphaloceles can be stable and may exhibit improvements over time. By allowing for natural growth and development, infants may achieve better surgical outcomes when intervention is ultimately necessitated.
Throughout the review, the authors highlight a variety of studies that corroborate the notion that immediate surgery is not always requisite or beneficial. They delve into the physiological adaptations that can occur during the initial months of life—periods characterized by increased tissue elasticity and abdominal cavity expansion. These factors can potentially facilitate surgery in a less urgent context, minimizing risks associated with premature interventions.
The review also emphasizes the importance of individualized patient care, where each case is assessed on its own merits. Factors such as the size of the omphalocele, the presence of other congenital anomalies, and the infant’s overall health significantly influence the timing decisions for surgical repair. This nuanced approach underscores the collaborative nature of neonatal care, involving surgeons, pediatricians, and neonatologists working together to craft personalized treatment plans.
In addition to surgical considerations, the psychological aspect of waiting treatments is discussed extensively. Waiting can be emotionally taxing for families, who may grapple with uncertainty and fear for their child’s health. The review highlights the necessity for robust support systems for families and emphasizes the need for transparent communication between healthcare providers and parents. Ensuring that families are well-informed may mitigate some of the emotional burdens associated with prolonged waiting periods.
Moreover, the investigators evaluated various outcomes linked to the conservative management of giant omphaloceles. They drew comparisons between surgical intervention groups and those managed conservatively. Interestingly, preliminary results indicated that children who underwent delayed surgery often had fewer complications and shorter recovery times. This revelation presents a paradigm shift in how clinicians might approach treatment, prompting healthcare systems to reevaluate protocols that were historically conservative in nature.
The systematic review also recognizes the technological advancements that have facilitated improved outcomes for these patients. With refined imaging techniques and better preoperative assessments, clinicians can now gauge the viability of bowel and other organs more accurately prior to surgery. These innovations enable a more tailored approach, allowing for better predictions regarding which infants may benefit from waiting to undergo surgical procedures.
Neonatology continues to evolve, and as new data becomes available, healthcare providers must remain adaptable in their methodologies. The contributions of Pan and colleagues play a pivotal role in guiding this evolution, embedding evidence-based practice within the standard care framework for managing giant omphaloceles. Their thorough examination serves as both a resource and a catalyst for new discussions regarding congenital abnormalities in neonates.
Moving forward, ongoing research is essential in refining our understanding of giant omphaloceles and optimizing treatment directions. Establishing multicenter collaborations could enhance the breadth of data collected and facilitate comparison across diverse patient cohorts, ultimately leading to a more robust evidence base. Such efforts must also consider variance in practices across geographic and cultural contexts, recognizing that treatment paradigms may shift globally.
In conclusion, the revolutionary insights garnered from this systematic review by Pan et al. illuminate a path forward in navigating the complexities of giant omphaloceles. By employing thoughtful evaluation and embracing a waiting treatment strategy, clinicians now have a promising alternative to more invasive surgical practices. The ongoing discourse surrounding this condition attests to the dynamic nature of medicine and the unyielding commitment to improving patient outcomes. As our grasp of the physiological and psychological ramifications of treatment choices enhances, the future for infants diagnosed with giant omphaloceles continues to brighten, offering hope for families and medical professionals alike.
Subject of Research: Giant Omphaloceles and the Waiting Treatment Model
Article Title: Clinical application and systematic review of waiting treatment for giant omphaloceles.
Article References:
Pan, R., Zhou, Z., Li, Z. et al. Clinical application and systematic review of waiting treatment for giant omphaloceles.
BMC Pediatr 25, 806 (2025). https://doi.org/10.1186/s12887-025-06206-2
Image Credits: AI Generated
DOI: 10.1186/s12887-025-06206-2
Keywords: Giant omphaloceles, waiting treatment, systematic review, neonatal care, congenital defects, surgical intervention, individualized care, psychological support.
Tags: clinical decision-making in surgerycongenital abdominal wall defectsgiant omphaloceles treatment strategiesinfant development outcomesinnovative patient care approaches.long-term complications in infantsmanagement of congenital defectsneonatology challengespsychological aspects of congenital conditionssurgical intervention timingsystematic review on omphaloceleswaiting treatment model efficacy