In the world of pediatric medicine, the understanding and treatment of intussusception—a condition where part of the intestine folds into another section—have seen significant advancements over the years. A prominent area of study is pneumatic intussusception reduction, a non-invasive technique that utilizes air pressure to correct this potentially life-threatening condition. Yet, clinicians have long grappled with the appropriate limits of air pressure to employ during this reduction process. Dr. E.L. Tung’s recent research provides fresh insights into why the threshold of 120 mmHg has become the standard in practice, sparking discussions and considerations within the medical community.
Intussusception primarily affects children, with the peak incidence occurring between six months and three years of age. The clinical presentation often includes abdominal pain, vomiting, and bloody stools, making timely and effective treatment critical. Traditionally, surgical intervention was the go-to solution for this distressing condition. However, the advent of pneumatic reduction techniques has offered a less invasive alternative, significantly altering management protocols. The application of controlled air pressure allows for the gentle rectification of the intestinal obstruction without the need for invasive surgery, minimizing recovery time and associated risks.
One major aspect that Dr. Tung explores in his article is the physiological basis behind the pressure limit of 120 mmHg for pneumatic intussusception reduction. This figure has emerged from a combination of observational data and clinical outcomes, underscoring the delicate balance of applying sufficient pressure to reduce the intussusception while avoiding the risk of intestinal perforation or other complications. The risks of exceeding this limit have been supported by various studies that indicate an increased incidence of adverse outcomes when higher pressures are utilized, prompting medical experts to solidify this threshold into clinical guidelines.
.adsslot_jhLJPWX8nx{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_jhLJPWX8nx{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_jhLJPWX8nx{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Moreover, the study highlights the need for careful monitoring during pneumatic reduction procedures. By employing a pressure of 120 mmHg, clinicians can better ensure the safety and comfort of their young patients. The importance of this limit cannot be overstated; exceeding it not only raises the risk of physical harm but also compromises the integrity of the therapeutic approach itself. Dr. Tung’s analysis includes vital parameters such as the average age of patients undergoing this technique, the duration of the procedure, and notable success rates, all anchored to the 120 mmHg guideline.
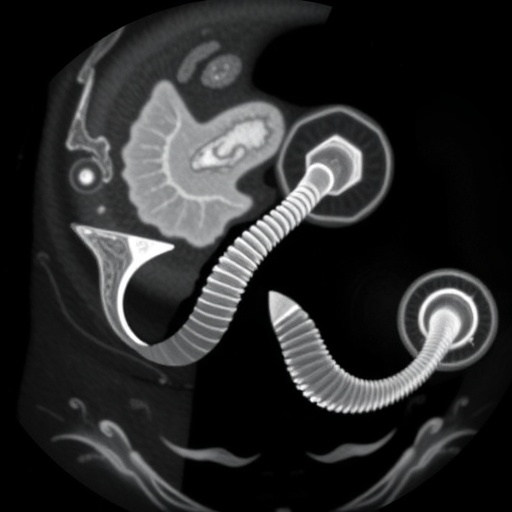
One of the underlying principles of pneumatic reduction is the physics of air pressure. When air is introduced into the rectum, it travels through the intestinal tract, creating a consistent and controlled force that enables the dislodging of the intussusception. Dr. Tung’s work synthesizes previous research and clinical anecdotes, examining how pressure dynamics play a crucial role in determining the success of this method. By maintaining a limit, clinicians also ensure that they do not compromise the vascularity of the bowel, which is paramount for preserving tissue integrity throughout the reduction process.
Dr. Tung’s research is particularly relevant given the increasing discussions surrounding pediatric healthcare practices and treatment efficacy. The reliance on pneumatic methods has surged, and with it, a natural inquiry into the thresholds of safe practice. The refinement of pneumatic intussusception techniques built upon empirical evidence and continually adjusted standards fosters a culture of safety first, ensuring that short-term interventions contribute positively to long-term outcomes in pediatric patients.
Patient safety continues to be a top priority, and with any procedure comes the necessity for informed consent—a teaching moment for families regarding the risks and benefits of pneumatic intussusception reduction. That dialogue plays an essential role in child-centric healthcare, where parents or guardians are often the primary decision-makers. Dr. Tung emphasizes that clear communication helps assuage parental anxieties while emphasizing the benefits realized by adhering to established pressure limits during reduction efforts.
Meanwhile, the confluence of technology and medicine has been instrumental in improving adherence to these standards. Modern medical imaging techniques allow for real-time visualization during pneumatic reductions, enhancing the accuracy of the procedure and informing clinicians about pressure management. The advent of ultrasound and fluoroscopy has provided non-invasive alternatives to anchor decisions during treatment, further validating the relevance of the 120 mmHg threshold.
It is essential to recognize that standards in medicine continuously evolve based on accumulating evidence and clinical experiences. Dr. Tung’s article not only substantiates the current 120 mmHg standard but also calls for further research focused on best practices for pneumatic intussusception reduction. As new technologies emerge, and with ongoing advocacy for patient-centered care, modifications and innovations in treatment paradigms are likely to emerge, informed by data such as Dr. Tung’s.
In conclusion, understanding the rationale behind the established limit of 120 mmHg serves as a benchmark for best practices in handling intussusception in pediatric patients. Dr. Tung’s research sheds light on a significant intersection of clinical efficacy and patient safety, bolstering the urgency of adhering to this standard. As pediatric radiology continues to advance, the insights drawn from this study will likely influence both current practices and future research endeavors—transforming the landscape of pediatric gastrointestinal emergencies as we know it.
Ultimately, ongoing discussions surrounding the pneumatic reduction of intussusception require a collective commitment from healthcare providers to ensure that children receive the safest, most effective care possible. By championing practices rooted in evidence and prioritizing patient safety, the medical community can inspire confidence among families and foster improved health outcomes for the pediatric population.
Subject of Research: The use of pneumatic pressure limits in intussusception reduction.
Article Title: Why do we use a limit of 120 mmHg for pneumatic intussusception reduction?
Article References:
Tung, E.L. Why do we use a limit of 120 mmHg for pneumatic intussusception reduction?.
Pediatr Radiol 55, 1745–1747 (2025). https://doi.org/10.1007/s00247-025-06319-x
Image Credits: AI Generated
DOI: July 2025
Keywords: Pneumatic intussusception reduction, pediatric medicine, air pressure limits, treatment safety, clinical guidelines.
Tags: 120 mmHg threshold for intussusceptionadvancements in pediatric gastroenterologyalternatives to surgical intervention for intussusceptionclinical implications of intussusception researchimpact of air pressure on intestinal healthnon-invasive treatment for intussusceptionpediatric emergency medicine practicespediatric intussusception managementpneumatic intussusception reduction techniquesreducing risks in pediatric intusssafe air pressure limits in intussusceptionunderstanding intussusception symptoms in children