In a significant advancement poised to transform the clinical management of non-small cell lung cancer (NSCLC), researchers have developed a predictive model utilizing computed tomography (CT) radiomics to forecast brain metastasis and overall prognosis in affected patients. This breakthrough leverages the power of imaging data combined with clinical indicators, enabling physicians to anticipate disease progression with remarkable accuracy. The study, published in BMC Cancer, introduces a sophisticated algorithm that integrates radiomics features extracted from chest CT scans, establishing a new frontier in personalized cancer care.
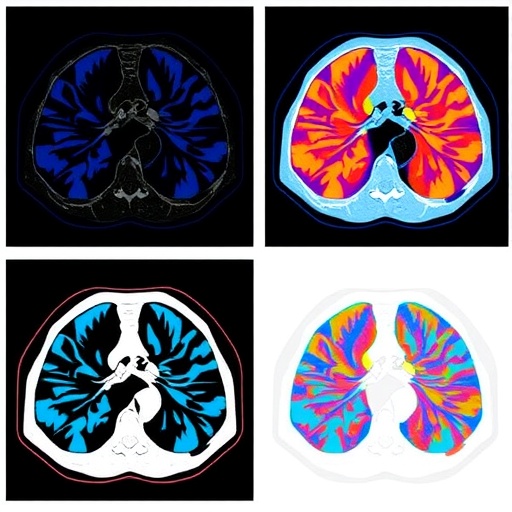
NSCLC remains a leading cause of cancer mortality globally, in large part due to its high propensity for brain metastases. These secondary tumors dramatically worsen patient outcomes and present therapeutic challenges, often emerging silently before clinical detection. Traditional prognostic methods have been limited by their reliance on clinical and pathological factors alone, which fail to capture the intricate tumor heterogeneity. By harnessing radiomics—a technique that transforms radiographic images into high-dimensional, quantifiable data—the novel model captures subtle imaging biomarkers indicative of metastatic potential.
The study analyzed chest CT scans from 215 NSCLC patients prior to any treatment intervention, alongside comprehensive clinical datasets such as lymph node status, lymphocyte percentages, and biochemical markers including neuron-specific enolase (NSE) levels. Radiomic features were meticulously extracted from lung window settings of CT images, encompassing texture, shape, and intensity parameters. This allowed for the computation of a radiomics score (Radscore), serving as a numerical representation of the tumor’s biological behavior.
.adsslot_8lk3Qa5JSv{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_8lk3Qa5JSv{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_8lk3Qa5JSv{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
A rigorous feature selection process identified key radiomics characteristics most predictive of brain metastasis. Subsequently, multiple predictive models were compared: a radiomics-only model, a clinical-only model, and a combined model merging both data types. The combined model demonstrated superior performance, achieving an area under the curve (AUC) of 0.849 in the training cohort and 0.816 in the validation cohort for brain metastasis prediction. These metrics outperform existing conventional strategies, indicating the model’s robust generalizability.
Beyond metastasis prediction, the investigators evaluated prognostic implications for patients already harboring brain metastases. Multivariate Cox regression analysis revealed that the number of brain metastases, presence of distant metastases to other organs, and elevated C-reactive protein (CRP) levels were independent predictors of survival outcomes. Importantly, calibration curves confirmed strong concordance between predicted survival probabilities and observed data, underscoring the model’s clinical reliability.
The research team further developed a nomogram—a visual predictive tool—derived from the joint clinical-radiomics model. This user-friendly instrument enables clinicians to input individual patient parameters, providing tailored risk assessments that can influence therapeutic decisions and surveillance strategies. Integration of such tools into routine oncology practice could refine patient stratification, identifying high-risk cases that may benefit from intensified treatment or closer monitoring.
This innovation exemplifies the broader trend in oncology toward precision medicine, where data-driven insights guide individualized management. By capturing the spatial heterogeneity and microenvironmental complexity of NSCLC tumors through non-invasive imaging, CT radiomics offers a window into tumor biology that surpasses biopsy limitations. It also offers a scalable and repeatable method for longitudinal patient evaluation.
However, developing such models requires overcoming technical challenges, including standardizing image acquisition protocols and addressing variability across scanners. The study acknowledges these hurdles and emphasizes the need for multicenter validation to ensure widespread applicability. Moreover, incorporating artificial intelligence and machine learning may further enhance the predictive ability and automate feature extraction, accelerating clinical translation.
The utilization of biomarkers such as NSE and lymphocyte percentage within the model underscores the synergy between imaging and molecular indicators. NSE, traditionally associated with neuroendocrine activity, suggests possible biological pathways underpinning brain metastasis propensity. Concurrently, inflammatory markers like CRP highlight the role of systemic factors in influencing prognosis, reflecting the complex interplay between tumor and host.
Importantly, the model’s predictive power surpasses what could be achieved through clinical variables alone, highlighting the added value of radiomics. This could prompt a paradigm shift where imaging data are not merely diagnostic but prognostic assets, reshaping oncology workflows. For patients, this means potential earlier interventions, optimized therapeutic regimens, and improved quality of life.
While the promising results lay foundational work, further research should explore integration with other modalities such as PET imaging or genomic profiling to develop multimodal predictive frameworks. Additionally, extending analyses to other metastatic sites could broaden the clinical impact. Patient-centric studies will also be critical to evaluate the model’s real-world effectiveness and acceptance.
Overall, this study is a landmark demonstration of how CT radiomics can move beyond detection to prognosis, offering valuable insights into NSCLC’s metastatic trajectory. It paves the way for personalized oncology strategies powered by advanced imaging analytics, holding the promise to improve survival outcomes and transform patient care.
As cancer treatment evolves into an era driven by big data and computational technology, such interdisciplinary research efforts are essential. The fusion of radiology, oncology, bioinformatics, and clinical expertise heralds a future where predictive modeling enhances decision-making and tailors interventions at the individual level.
The integration of predictive radiomics into clinical pathways may soon become standard practice, revolutionizing how oncologists anticipate disease course and tailor patient management. This progress underscores the critical importance of harnessing existing clinical data with innovative computational methods to unlock new prognostic dimensions.
Ultimately, this CT radiomics-based model signifies a vital step toward conquering the complexities of NSCLC brain metastases. It offers hope that precision prognostication can become a realistic and actionable tool in the ongoing fight against lung cancer’s deadliest sequelae.
Subject of Research: Prognostic prediction of brain metastasis and survival outcomes in non-small cell lung cancer patients using CT radiomics-based models.
Article Title: Application of prediction model based on CT radiomics in prognosis of patients with non-small cell lung cancer.
Article References:
Peng, Z., Wang, Y., Qi, Y. et al. Application of prediction model based on CT radiomics in prognosis of patients with non-small cell lung cancer. BMC Cancer 25, 1273 (2025). https://doi.org/10.1186/s12885-025-14544-8
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14544-8
Tags: advanced cancer prognostic modelsbrain metastasis predictioncancer mortality factorschest CT scan analysisclinical indicators in cancerCT radiomics in lung cancerimaging biomarkers in NSCLCnon-small cell lung cancer prognosispersonalized cancer care strategiespredictive modeling in oncologyradiomic features extraction techniquestumor heterogeneity assessment