Study suggests spatial relationship between COVID-19 mortality and population-level health factors
Credit: Kandula S and Shaman J, 2021, PLOS Medicine,
CC-BY 4.0 (https://creativecommons.org/licenses/by/4.0/)
An estimated 43 percent of the variability in U.S. COVID-19 mortality is linked with county-level socioeconomic indicators and health vulnerabilities, with the strongest association seen in the proportions of people living with chronic kidney disease and living in nursing homes. The study by Columbia University Mailman School of Public Health researchers suggests that allocating vaccines based on these factors could help minimize severe outcomes, particularly deaths. Results are published in the open-access journal PLOS Medicine.
“It is well known that COVID-19 deaths are concentrated in communities with underlying health and socioeconomic vulnerabilities. Our study estimates increase in risk from some of the key health and socioeconomic characteristics in the U.S.,” says Sasikiran Kandula, MS, the study’s first author and senior staff associate in the Department of Environmental Health Sciences at Columbia Mailman School of Public Health.
“This information can guide the distribution of vaccines, particularly in parts of the world where vaccine supply is limited, in order to get them to communities where they are needed most,” adds senior author Jeffrey Shaman, PhD, professor of environmental health sciences at Columbia Mailman School of Public Health.
Currently, COVID-19 vaccination strategies in the United States are informed by individual characteristics such as age and occupation. The effectiveness of population-level health and socioeconomic indicators to determine risk of COVID-19 mortality is understudied.
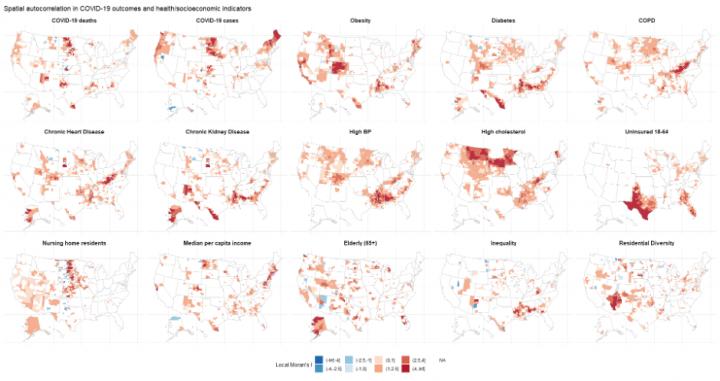
To test their hypothesis that health and socioeconomic indicators can accurately model risk of COVID-19 mortality, Shaman and Kandula extracted county-level estimates of 14 indicators associated with COVID-19 mortality from public data sources. They then modeled the proportion of county-level COVID-19 mortality explained by identified health and socioeconomic indicators, and assessed the estimated effect of each predictor.
They found that 43 percent of variability in U.S. COVID-19 mortality can be traced to 9 county-level socioeconomic indicators and health vulnerabilities after adjusting for associations in deaths rates between adjacent counties.
Among health indicators, mortality is estimated to increase by 43 per thousand residents for every 1 percent increase in the prevalence of chronic kidney disease, and by 10 for chronic heart disease, 7 for diabetes, 4 for COPD, 4 for high cholesterol, 3 for high blood pressure and 3 for obesity prevalence respectively. Among socioeconomic indicators, mortality is estimated to increase by 39 deaths per thousand for every 1 percent increase in percent living in nursing homes, and by 3 and 2 for each 1 percent increase in the percentage of the population who are elderly (65+ years) and uninsured 18-64-year-olds, respectively. Mortality rate is estimated to decrease by 2 for every thousand dollar increase in per capita income.
Although the research suggests a correlation between health and socioeconomic indicators and COVID-19 mortality, the study was limited by lags in reporting COVID-19 cases and deaths, and therefore these may have been underestimated.
###
The study is funded in part by a grant from the National Science Foundation (DMS-2027369) and a gift from the Morris-Singer Foundation to JS. The authors report the following competing interests: JS and Columbia University disclose ownership of SK Analytics and JS discloses personal fees from BNI (Business Network International). SK consulted for SK Analytics.
Media Contact
Tim Paul
[email protected]
Related Journal Article
http://dx.




