Clues sought for why 1 in 5 pediatric cancer survivors develop heart failure
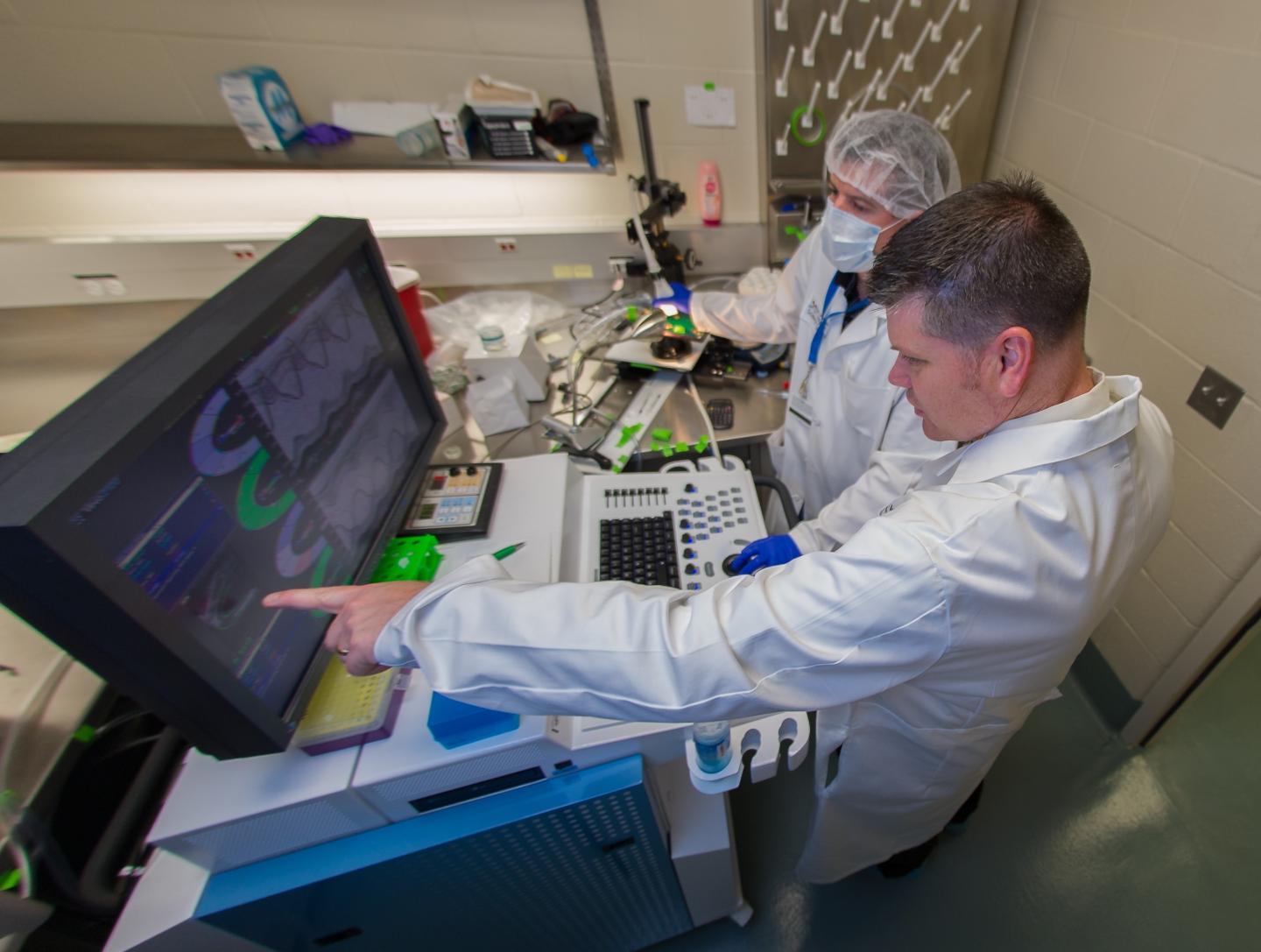
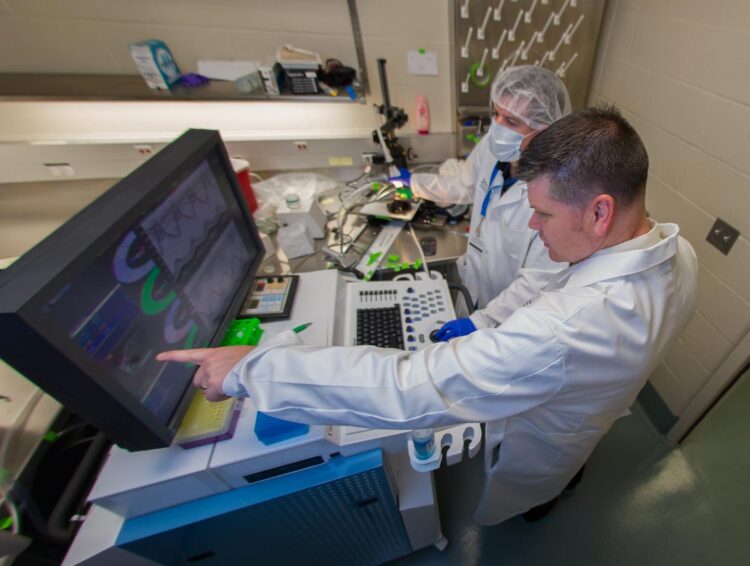
Credit: UT Health San Antonio
Cancer chemotherapy changes the function of cells that repair heart injury, researchers at The University of Texas Health Science Center at San Antonio (UT Health San Antonio) discovered. Twenty percent of children treated with drugs called anthracyclines go on to suffer heart failure later in life.
The journal PLOS ONE published the results Sept. 22 during Childhood Cancer Awareness Month.
“We don’t fully understand why some children who are exposed to anthracycline therapy develop these problems with the heart three to four decades later,” said study senior author Gregory Aune, MD, PhD, of the Greehey Children’s Cancer Research Institute at UT Health San Antonio.
“The cardiac fibroblast, which acts as a sort of caretaker cell in the heart and other tissues of the body, has not been well studied in relation to this problem,” said Dr. Aune, a pediatric oncologist in the Joe R. and Teresa Lozano Long School of Medicine. “We believe damage to these cells may contribute to effects seen in childhood cancer survivors when they become adults.”
The group is studying how a tumor-suppressor gene called p53, which protects genes from damage, impacts the response of cardiac fibroblasts to anthracyclines. In mouse cells lacking p53 that were exposed to the drug, fibroblast function was altered, Dr. Aune said.
“Normal fibroblasts have the ability to migrate, presumably to help repair injury in the heart,” said Trevi Mancilla, PhD, first author of the report. “Cardiac fibroblasts treated with anthracycline show less migration. We have not established whether or not that is detrimental.”
Dr. Mancilla is a student in the South Texas Medical Scientist Training Program, which is the MD-PhD dual-degree program at UT Health San Antonio, and is also in the university’s Department of Cellular and Integrative Physiology.
Pediatric oncologists give lower doses of anthracycline chemotherapy than when the drugs were introduced four decades ago. Cases of heart failure brought on acutely by the therapy are now rare.
“Although we don’t see heart failure or a decline in heart function, that doesn’t necessarily mean cells in the heart are not being damaged,” Dr. Aune said.
Other cell types in the heart include cardiomyocytes, which enable the heart to contract; endothelial cells, which line blood vessels; and immune cells, which respond to injury or infection.
But it is the fibroblasts that have the Aune lab’s attention.
“The overarching hypothesis we have in the lab is that damage to this cell population, the cardiac fibroblast, isn’t innocuous,” Dr. Aune said. “These cells can have their properties changed by exposure to gene-damaging agents. And then theoretically over time, that may be one contributor to the late effects that we see.”
“That might translate into an inability to respond to insults such as high blood pressure or heart attacks, because fibroblasts are so important in dealing with injury,” Dr. Mancilla said.
###
Doxorubicin-induced p53 interferes with mitophagy in cardiac fibroblasts
Trevi R. Mancilla, Logan R. Davis, Gregory J. Aune
First published: Sept. 22, 2020, PLOS ONE
https:/
The Long School of Medicine at The University of Texas Health Science Center at San Antonio is named for Texas philanthropists Joe R. and Teresa Lozano Long. The school is the largest educator of physicians in South Texas, many of whom remain in San Antonio and the region to practice medicine. The school teaches more than 900 students and trains 800 residents each year. As a beacon of multicultural sensitivity, the school annually exceeds the national medical school average of Hispanic students enrolled. The school’s clinical practice is the largest multidisciplinary medical group in South Texas with 850 physicians in more than 100 specialties. The school has a highly productive research enterprise where world leaders in Alzheimer’s disease, diabetes, cancer, aging, heart disease, kidney disease and many other fields are translating molecular discoveries into new therapies. The Long School of Medicine is home to a National Cancer Institute-designated cancer center known for prolific clinical trials and drug development programs, as well as a world-renowned center for aging and related diseases.
The University of Texas Health Science Center at San Antonio, also referred to as UT Health San Antonio, is one of the country’s leading health sciences universities and is designated as a Hispanic-Serving Institution by the U.S. Department of Education. With missions of teaching, research, patient care and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have graduated more than 37,000 alumni who are leading change, advancing their fields, and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit http://www.
Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.
To see how we are battling COVID-19, read inspiring stories on Impact.
Media Contact
Will Sansom
[email protected]
Original Source
https:/
Related Journal Article
http://dx.