Promising target for blood-based diagnostic test
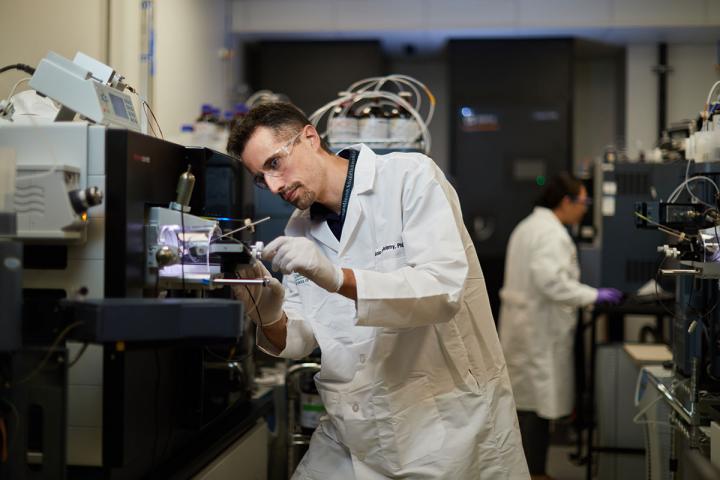
Credit: Matt Miller
Two decades or more before symptoms arise, plaques of a sticky protein called amyloid begin forming in the brains of people later diagnosed with Alzheimer’s disease. Researchers at Washington University School of Medicine in St. Louis have shown that levels of a specific protein in the blood rise as amyloid plaques form in the brain. This protein can be detected in the blood of people who have yet to show signs of forgetfulness or confusion, making it a promising blood test to diagnose Alzheimer’s before symptoms appear.
The findings are published July 28 in the Journal of Experimental Medicine.
“The finding of a unique tau species that is closely linked to changes caused by amyloid plaques will help to identify and predict people who have or will likely develop Alzheimer’s disease,” said senior author Randall J. Bateman, MD, the Charles F. and Joanne Knight Distinguished Professor of Neurology. “This will greatly accelerate research studies, including finding new treatments, as well as improving diagnosis in the clinic with a simple blood test.”
Alzheimer’s disease begins with a silent phase lasting two decades or more during which amyloid plaques slowly collect in the brain without causing obvious cognitive problems. For decades, researchers have been searching for an easy and affordable way to identify people in the so-called preclinical stage so that, once effective drugs are available, they could be treated and, ideally, never develop symptoms at all.
Positron emission tomography (PET) brain scans can identify people with amyloid plaques, but they are too time-consuming and expensive to be widely used for screening or diagnosis. Bateman and colleagues already are working on a blood test for amyloid that has shown promise at distinguishing people with amyloid in their brains from those without. But first author Nicolas Barthélemy, PhD, an instructor in neurology, Bateman and others realized that a different Alzheimer’s protein – tau – also may be useful for identifying which people have amyloid plaques silently gathering in their brains.
Barthélemy and Bateman previously had discovered that people with amyloid plaques tend to have certain forms of tau in the cerebrospinal fluid that surrounds their brains and spinal cords. Sampling the cerebrospinal fluid requires a spinal tap, which some participants are reluctant to undergo, but proteins in the cerebrospinal fluid can spill over into the blood, which is easier to obtain. If these specific forms of tau could be found in a person’s blood, they reasoned, that might be an indication that the person has the consequences of amyloid plaques in his or her brain.
To evaluate this possibility, the researchers analyzed blood samples and brain scans from 34 people participating in Alzheimer’s research studies at the university’s Charles F. and Joanne Knight Alzheimer’s Disease Research Center. Nineteen of the participants had no amyloid in their brains, five had amyloid but no cognitive symptoms, and 10 had amyloid and cognitive symptoms. The researchers used a technique known as mass spectrometry to identify and measure the different forms of tau in the blood samples. They found that levels of a form of tau known as phosphorylated tau 217 correlated with the presence of amyloid plaques in the brain. People with amyloid in their brains had two to three times more of the protein in their blood than people without amyloid. These high levels were evident even in people with no signs of cognitive decline.
To verify their findings, the researchers repeated the analysis in a separate group of 92 people: 42 with no amyloid, 20 with amyloid but no cognitive symptoms, and 30 with amyloid and symptoms. In this analysis, levels of phosphorylated tau 217 in the blood correlated with the presence of amyloid in the brain with more than 90% accuracy. When the researchers looked only at people with no cognitive symptoms, blood levels of phosphorylated tau 217 distinguished those in the early, asymptomatic stage of Alzheimer’s disease from healthy people with 86% accuracy.
“This is just an exploratory study, but we think phosphorylated tau 217 is a promising target for an early diagnostic test,” Barthélemy said. “There was a large difference between the amyloid-positive and amyloid-negative groups, even amongst people who were cognitively normal. We did have to use a large volume of blood in this study, but we’re working on reducing the volume. Once we improve the way we are preparing and concentrating the sample, we will be a step closer to developing a tau-based blood test that can identify people at risk of developing Alzheimer’s dementia before symptoms arise.”
###
Media Contact
Judy Martin Finch
[email protected]
Related Journal Article
http://dx.




