Researchers take a step closer to 3D printing living tissues in patients
Credit: Ohio State University
(LOS ANGELES) – In the TV series Westworld, human body parts are built on robotic frames using 3D printers. While still far from this scenario, 3D printers are being increasingly used in medicine. For example, 3D printing can be used to produce parts of the body such as orthopedic joints and prosthetics, as well as portions of bone, skin and blood vessels. However, the majority of these tissues are created in an apparatus outside of the body and surgically implanted. Such a procedure may involve making large surgical incisions, posing the added risk of infection and increased recovery time for the patient. And since there is a time lapse between when the tissue is created and when it is implanted in the patient, further complications may occur. To prevent these complications, a team of scientists have developed a technology to print tissues directly in the body.
There are two basic components needed to produce an engineered tissue: (1) a fluid-like “bio-ink” that consists of a framework material mixed with living cells, and (2) growth factors to help the cells grow and develop into regenerated tissue. When developing tissues for direct implantation into the body, there are other things to consider: the construction of tissue would have to be conducted at body temperature (37°C), the tissue needs to be attached effectively to soft, live organ tissue and any procedural steps should not be harmful to the patient. One such harmful step in current methods is the application of harmful UV light necessary to solidify the constructed tissue.
A collaboration among Ali Khademhosseini, Ph.D., Director and CEO of the Terasaki Institute, David J Hoelzle, Ph.D., from the Ohio State University Department of Mechanical and Aerospace Engineering and Amir Sheikhi, Ph.D. from the Pennsylvania State University Department of Chemical Engineering, has produced a specially-formulated bio-ink designed for printing directly in the body.
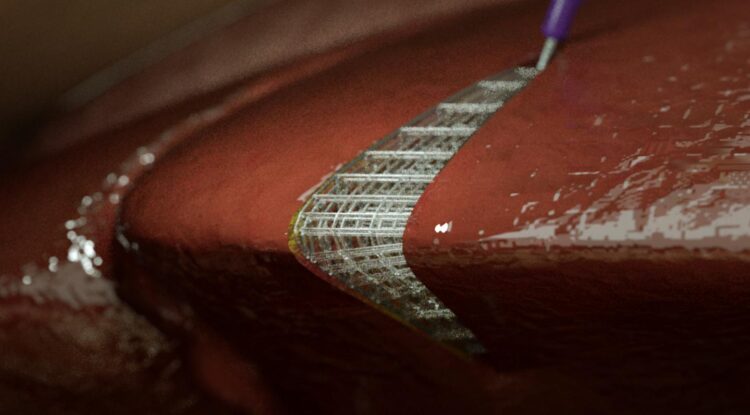
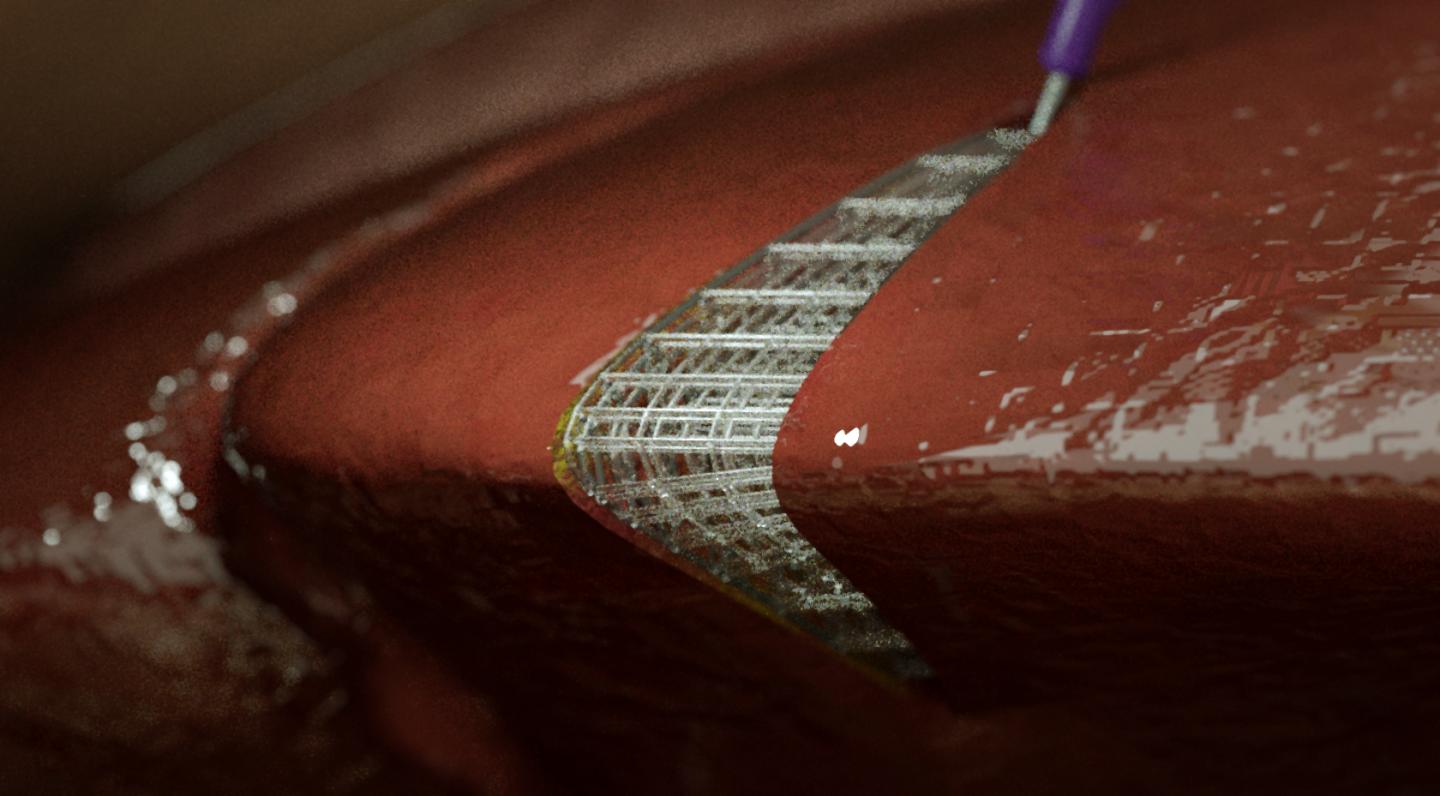
“This bio-ink formulation is 3D printable at physiological temperature, and can be crosslinked safely using visible light inside the body.” said first author Ali Asghari Adib, Ph.D. In order to build the tissue, they used robotic 3D printing, which uses robotic machinery affixed with a nozzle. Bio-ink may be dispensed through the nozzle, much like an icing tube squeezes out writing gel, only in a highly-precise, programmable manner.
The team also worked on methods to attach pieces of the tissue formed with this bio-ink onto soft surfaces. In experiments attempting to attach the tissue onto pieces of raw chicken strips and agarose, the team employed a unique interlock technique using the robotic 3D printer and their specially-formulated bio-ink. The nozzle tip was modified to be able to penetrate the soft surfaces and fill the punctured space with bio-ink as it withdrew; this created an anchor for the tissue construct. As the nozzle tip reached the surface, it dispensed an additional blob of bio-ink to “lock in” the anchor. “The interlocking mechanism enables stronger attachments of the scaffolds to the soft tissue substrate inside the patient body,” said Asghari Adib.
Such improvements in tissue engineering are instrumental in providing lower-risk, minimally-invasive laparoscopic options for procedures such as the repair of tissue or organ defects, engineering/implanting patches to enhance ovarian function, or creating bio-functional hernia repair meshes. Such options would be safer for the patient, save time and be more cost-effective. Further modifications in tissue engineering design and the adjustment of other conditions may increase the potential for customization, thus leading the way to limitless possibilities for enhancing patient health.
“Developing personalized tissues that can address various injuries and ailments is very important for the future of medicine. The work presented here addresses an important challenge in making these tissues, as it enables us to deliver the right cells and materials directly to the defect in the operating room,” said Khademhosseini, “This work synergizes with our Personalized Implant Technology Platform at the Terasaki Institute which aims to develop approaches that address the variability in tissue defects in patients.”
###
Additional authors on the article include Melika Shahhosseini, Andrej Simeunovic, Ph.D., Shuai Wu, Carlos Castro, Ph.D., and Ruike Zhao, Ph.D. Financial support came from the National Science Foundation under grants CMMI-1552358 CAREER and IIP-1919204.
PRESS CONTACT
Stewart Han, [email protected], +1 818-836-4393
Terasaki Institute for Biomedical Innovation
The Terasaki Institute for Biomedical Innovation (terasaki.org) is a non-profit research organization that invents and fosters practical solutions that restore or enhance the health of individuals. Research at the Terasaki Institute leverages scientific advancements that enable an understanding of what makes each person unique, from the macroscale of human tissues down to the microscale of genes, to create technological solutions for some of the most pressing medical problems of our time. We use innovative technology platforms to study human disease on the level of individual patients by incorporating advanced computational and tissue-engineering methods. Findings yielded by these studies are translated by our research teams into tailored diagnostic and therapeutic approaches encompassing personalized materials, cells and implants with unique potential and broad applicability to a variety of diseases, disorders and injuries.
The Institute is made possible through an endowment from the late Dr. Paul I. Terasaki, a pioneer in the field of organ transplant technology.
Media Contact
Stewart Han
[email protected]
Original Source
https:/
Related Journal Article
http://dx.