Next-generation gene sequencing finds mutations in patients resistant to PSMA-targeting therapy
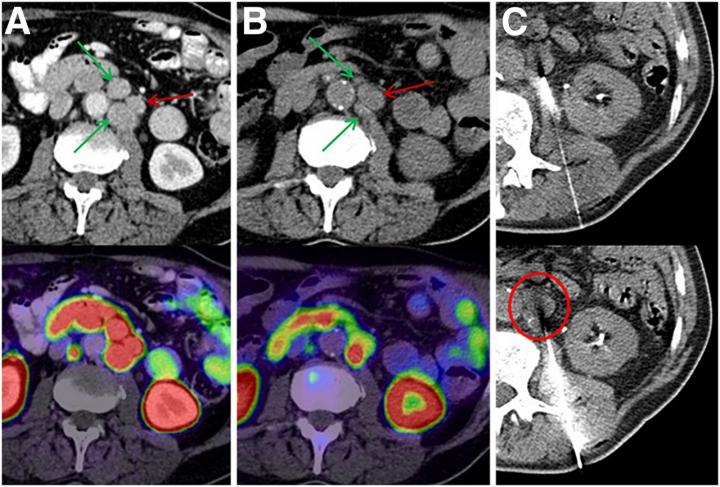
Credit: Images created by C Kratochwil and CP Heussel et al., University Hospital Heidelberg, Germany.
Reston, VA–Prostate cancer patients who do not respond well to PSMA-targeted therapy often have potentially treatable mutations in their DNA damage-repair genes, according to research published in the May issue of The Journal of Nuclear Medicine. In an exploratory study using a relatively new technique–targeted next-generation gene sequencing–researchers found mutations in six out of seven patients with metastatic castration-resistant prostate cancer who did not respond to prostate-specific membrane antigen (PSMA)-targeted radiopharmaceutical therapy despite sufficient PSMA expression in their tumors.
Prostate-specific membrane antigen-targeting α-radiation therapy (PSMA-TAT) with 225Ac-PSMA-617 is an emerging and promising approach to treating metastatic castration-resistant prostate cancer. However, a reported 37 percent of patients respond poorly to this therapy even though they have sufficient PSMA expression. Preclinical and early studies suggest that particular DNA damage-repair-associated gene mutations can either increase or decrease the radiosensitivity of prostate cancers and may influence a patient’s response to radiopharmaceutical therapy.
“Given the important role of DNA damage-repair gene alterations, we sought to evaluate the frequency of these defects in patients with an insufficient response to 225Ac-PSMA-617 therapy with next-generation gene sequencing,” said Clemens Kratochwil, MD, supervising physician for radionuclide therapy at Heidelberg University Hospital in Heidelberg, Germany. “A relatively new technique, targeted next-generation sequencing, allows rapid analysis of an individual tumor’s genome. Theoretically, such information can be predictive as to whether a patient has an increased probability to benefit from one specific treatment or combination therapy.”
From a group of 60 patients treated with 225Ac-PSMA-617 PSMA-TAT, researchers identified 10 patients with a poor therapy response despite sufficient PSMA expression. CT-guided biopsies were obtained from seven of the 10 patients and then validated with histopathology and immunostaining. Biopsy specimens were analyzed with two separate targeted next-generation-sequencing panels to detect mutations in 37 genes involved in DNA-damage recognition, checkpoint signaling or DNA-damage repair.
In the seven biopsy specimens, researchers found a total of 15 whole-gene deletions, deleterious mutations and presumably deleterious mutations. Loss of function alterations were found more than once in TP53, ATM and CHEK2, with one patient even having a co-mutation of TP53 and CHEK2. Further loss-of-function mutations or whole-gene deletions were detected once in the analyzed sample set for BRCA1, BRCA2, PMS1, NBN, MSH2, MSH6, PALB2 and FANCB, respectively. For some other alterations found in ATM, BRCA1, MSH2, SLX4, ERCC and various FANC genes, it was not clear whether they negatively affected its function or were non-pathological variants as part of the normal human diversity.
“Whether the efforts and costs of next-generation sequencing are warranted in a dedicated clinical situation will depend on several factors,” noted Kratochwil. “First, the mutation must be druggable in order to be led to a change in therapeutic management. Second, if the mutations are very rare, then sophisticated testing would not be cost- or time-effective. Lastly, if many patients were found to have comparable mutations, individual testing could be avoided and a one-size-fits-all approach could be applied. The significance of this preliminary work is in guiding of further research, and our findings will likely lead to a change of research practice in the near future.”
He continued, “Once it can be confirmed that a large number of patients receiving PSMA-TAT are simultaneously harboring potentially druggable mutations in genes that are causal related to radio-sensitivity, then clinical evaluation (and hopefully one day routine application) of combination therapies with the potential of over-additive efficacy will become available.”
###
This study was made available online in October 2019 ahead of final publication in print in May 2020.
The authors of “Patients Resistant Against PSMA-Targeting α-Radiation Therapy Often Harbor Mutations in DNA Damage-Repair- Associated Genes” include Clemens Kratochwil, Frederik L. Giesel and Hendrik Rathke, Department of Nuclear Medicine, Heidelberg University Hospital, Heidelberg, Germany; Claus-Peter Heussel, Thorax Centre, Department of Interventional and Diagnostic Radiology, Heidelberg University Hospital, Heidelberg, Germany; Daniel Kazdal, Volker Endris, Jonas Leichsenring and Albrecht Stenzinger, Institute of Pathology, Heidelberg University Hospital, Heidelberg, Germany; Cathleen Nientiedt, Department of Medical Oncology, National Center for Tumor Diseases, Heidelberg, Germany, and Section of Molecular Urooncology, Department of Urology, Heidelberg University Hospital, Heidelberg, Germany; Frank Bruchertseifer and Alfred Morgenstern, Directorate for Nuclear Safety and Security, European Commission-Joint Research Centre, Karlsruhe, Germany; Maximilian Kippenberger, Section of Molecular Urooncology, Department of Urology, Heidelberg University Hospital, Heidelberg, Germany; Markus Hohenfellner, Department of Urology, Heidelberg University Hospital, Heidelberg, Germany; Uwe Haberkorn, Department of Nuclear Medicine, Heidelberg University Hospital, Heidelberg, Germany, and Clinical Cooperation Unit Nuclear Medicine, German Cancer Research Center, Heidelberg, Germany; and Stefan Duensing, Section of Molecular Urooncology, Department of Urology, Heidelberg University Hospital, Heidelberg, Germany, and Department of Urology, Heidelberg University Hospital, Heidelberg, Germany.
Please visit the SNMMI Media Center for more information about molecular imaging and precision imaging. To schedule an interview with the researchers, please contact Rebecca Maxey at (703) 652-6772 or [email protected].
About the Society of Nuclear Medicine and Molecular Imaging
The Journal of Nuclear Medicine (JNM) is the world’s leading nuclear medicine, molecular imaging and theranostics journal, accessed close to 10 million times each year by practitioners around the globe, providing them with the information they need to advance this rapidly expanding field. Current and past issues of the journal can be found online at http://jnm.
JNM is published by the Society of Nuclear Medicine and Molecular Imaging (SNMMI), an international scientific and medical organization dedicated to advancing nuclear medicine and molecular imaging–precision medicine that allows diagnosis and treatment to be tailored to individual patients in order to achieve the best possible outcomes. For more information, visit http://www.
Media Contact
Rebecca Maxey
[email protected]
Original Source
http://www.
Related Journal Article
http://dx.




