Mini grant from the UC College of Medicine helps team investigate pathogen’s mechanis
Credit: Colleen Kelley/UC Creative + Brand
Researchers are finding about half of all patients with COVID-19 admitted to an intensive care unit have heart damage.
“Patients with heart damage are at risk for life-threatening irregularities of the heart rhythm,” says Richard Becker, director of the University of Cincinnati Heart, Lung and Vascular Institute and a UC Health cardiologist. “In some instances, the heart rhythm abnormalities will occur following discharge from the ICU and in other cases after hospital discharge.”
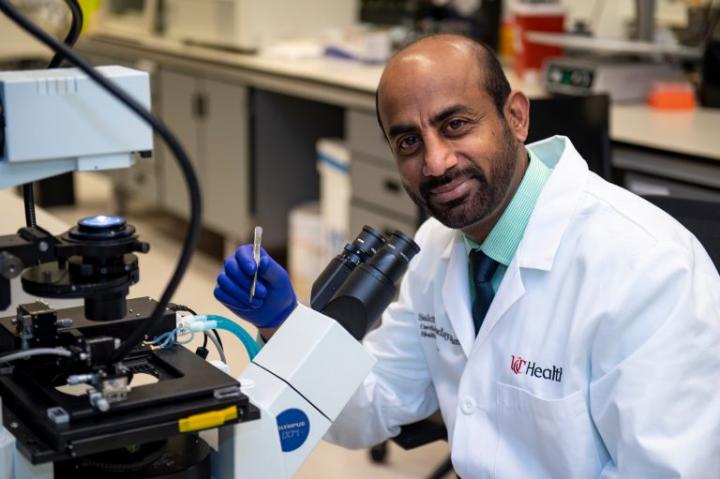
The troubling trend of heart injury for COVID-19 patients is why a team of UC researchers is using a $50,000 mini grant from the UC College of Medicine to understand how the SARS-CoV-2 virus, the pathogen of COVID-19, impacts heart cells. Sakthivel Sadayappan, PhD, the grant’s principal investigator, Becker and Donald Lynch, MD, are leading this effort.
Researchers will convert stem cells in laboratory petri dishes into heart cells to test hypotheses about the pathogen’s mechanism, says Sadayappan, a professor and associate chair of research in the UC Department of Internal Medicine. The virus can attach to heart cells through specific connectors known as spike proteins, which give the virus its spiked appearance.
The researchers hope to learn how interferons activated in COVID-19 infections defend the heart and whether the SARS-CoV-2 spike protein binding to a specific receptor causes cardiomyocyte injury, says Sadayappan. They will also test the heart-specific protective effects of several medications being studied in the treatment of COVID-19 patients.
“This is a critical project that has to happen as soon as possible given our current understanding of the heart and COVID-19 in the midst of an ongoing pandemic,” says Sadayappan. “The seed money from the College of Medicine will allow us to collect preliminary data that will assist in securing additional funding to advance our research findings.”
Becker says the attachment of the virus to the heart may cause injury in several unique ways and a release of troponin that can be measured in the blood.
“Because any injury to the heart causes troponin levels to rise, we will measure troponin attached to virus spike proteins together in complex,” adds Becker. “This may be the first diagnostic test specific for COVID-19 related heart injury.”
Lynch, an assistant professor in the UC College of Medicine and a UC Health cardiologist, says the research will hopefully lead to the discovery of novel plasma biomarkers that can predict early signs of severe cardiac injury, arrhythmias and sudden cardiac death.
He says COVID-19 is affecting patients in ways that exacerbate pre existing racial and health inequalities in the United States. Reports of African American being disproportionately hit by COVID-19 deaths are linked to other health concerns including cardiovascular well-being.
Lynch cited statistics from the Centers for Disease Control and Prevention which show African Americans are 40% more likely to have hypertension, twice as likely to suffer from stroke and have higher rates of diabetes and obesity. In Ohio, African Americans have a 34% higher death rate from COVID-19, says Lynch.
“We need to further define how this virus injuries the heart or its electrical circuitry leading to adverse health outcomes for Ohio residents and beyond,” says Lynch.
###
Media Contact
Cedric Ricks
[email protected]
Original Source
https:/




