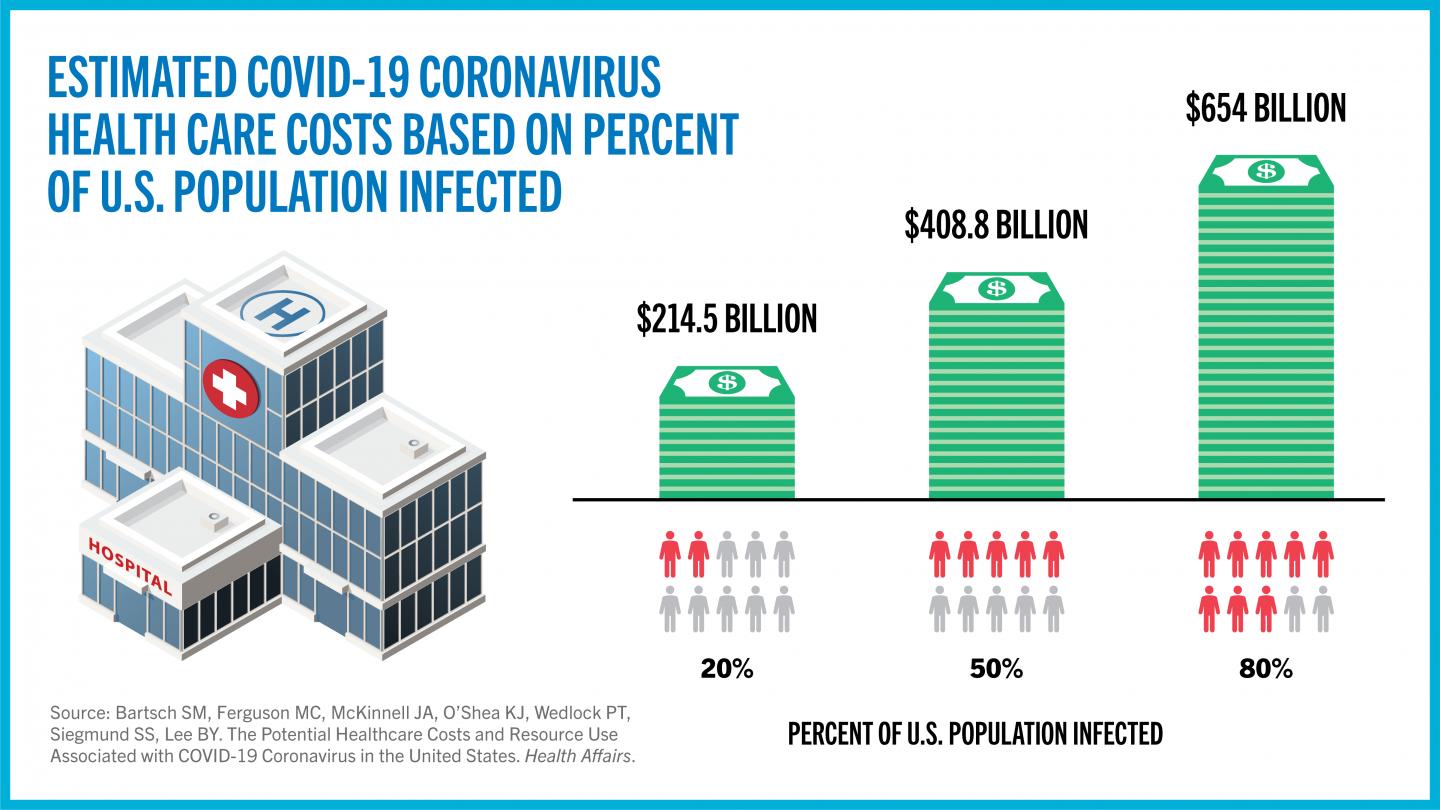
Study shows hospitalizations, ventilators, and other health resources that patients would require could cost $654 billion if a majority of the population gets infected
Credit: CUNY SPH
One of the major concerns about the COVID-19 coronavirus pandemic has been the burden that cases will place on the health care system. A new study published April 23 in the journal Health Affairs found that the spread of the virus could cost hundreds of billions of dollars in direct medical expenses alone and require resources such as hospital beds and ventilators that may exceed what is currently available. The findings demonstrate how these costs and resources can be cut substantially if the spread of COVID-19 coronavirus can be reduced to different degrees.
The study was led by the Public Health Informatics, Computational, and Operations Research (PHICOR) team at the City University of New York (CUNY) Graduate School of Public Health and Health Policy (CUNY SPH) along with the Infectious Disease Clinical Outcomes Research Unit (ID-CORE) at the Los Angeles Biomedical Research Institute, Harbor-UCLA Medical Center and Torrance Memorial Medical Center. The team developed a computer simulation model of the entire U.S. that could then simulate what would happen if different proportions of the population end up getting infected with the COVID-19 coronavirus. In the model, each infected person would develop different symptoms over time and, depending upon the severity of those symptoms, visit clinics, emergency departments, or hospitals. The resources each patient would require such as health care personnel time, medication, hospital beds, and ventilators would then be based on the health status of each patient. The model then tracks the resources invovled, the associated costs, and the outcomes for each patient.
For example, if 20 percent of the U.S. population were to become infected with the COVID-19 coronavirus, there would be an average of 11.2 million hospitalizations and 1.6 million ventilators used, costing an average of $163.4 billion in direct medical costs during the course of the infection. The study shows the factors that could push this amount up to 13.4 million hospitalizations and 2.3 million ventilators used, costing an average of $214.5 billion. If 50 percent of the U.S. population were to get infected with the COVID-19 coronavirus, there would be 27.9 million hospitalizations, 4.1 million ventilators used and 156.2 million hospital bed days accrued, costing an average of $408.8 billion in direct medical costs during the course of the infection. This increases to 44.6 million hospitalizations, 6.5 million ventilators used and 249.5 million hospital bed days (general ward plus ICU bed days) incurred, costing an average of $654 billion during the course of the infection if 80 percent of the U.S. population were to get infected. The significant difference in medical costs when various proportions of the population get infected show the value of any strategies that could reduce infections and, conversely, the potential cost of simply letting the virus run its course.
“Some have suggested herd immunity strategies for this pandemic,” explained Sarah Bartsch, project director at PHICOR and the study’s lead author. “These strategies consist of allowing people to get infected until herd immunity thresholds are reached and the virus can no longer spread. However, our study shows that such strategies could come at a tremendous cost.”
“This also shows what may occur if social distancing measures were relaxed and the country were to be ‘re-opened’ too early,” said CUNY SPH Professor Bruce Y. Lee, executive director of PHICOR and the study’s senior author. “If the virus is still circulating and the infection rates surge as a result, we have to consider the resulting health care costs. Such costs will affect the economy as well because someone will have to pay for them. Any economic argument for re-opening the country needs to factor in health care costs.”
The study shows how costly the COVID-19 coronavirus is compared to other common infectious diseases. For example, a single symptomatic COVID-19 coronavirus infection costs an average of $3,045 in direct medical costs during the course of the infection alone. This is four times higher than a symptomatic influenza case and 5.5 times higher than a symptomatic pertussis case. Factoring in the costs from longer lasting effects of the infection such as lung damage and other organ damage increased the average cost to $3,994.
“This is more evidence that the COVID-19 coronavirus is very different from the flu,” said Bartsch. “The burden on the health care system and the resources needed are very different.”
“Factoring in the costs incurred after the infection is over also adds to the costs. It is important to remember that for a proportion of the people who get infected, health care costs don’t end when the active infection ends,” Lee warned. “This pandemic will have its lasting effects and taking care of those who will suffer contuing problems is one of them.”
A continuing concern is that the U.S. health care system will become overloaded with the surge of COVID-19 coronavirus cases and will subsequently not have enough person-power, ventilators, and hospital beds to accommodate the influx of patients. This study shows that even when only 20 percent of the population gets infected, the current number of available ventilators and ICU beds will not be suffient. According to the Society of Critical Care Medicine, there are approximately 96,596 ICU beds and 62,000 full-featured mechanical ventilators in U.S., substantially lower than what would be needed when only 20 percent of the population gets infected.
“Of course, the actual capacity used will depend on the timing of when patients need them,” said Bartsch. “But showing that there are orders of magnitude differences between what is currently available and what may be needed is concerning.”
While health care professionals and public health officials have expressed concerns about ventilator and hospital bed shortages, the model can quantify in a more detailed manner what specifically will be required at different phases of the pandemic and what to expect when more people are infected.
###
“The Potential Health Care Costs and Resource Use Associated with COVID-19 Coronavirus in the United States” was written by Sarah M. Bartsch, Marie C. Ferguson, James A. McKinnell, Kelly J. O’Shea, Patrick T. Wedlock, Sheryl S. Siegmund and Bruce Y. Lee.
This work was supported in part by CUNY SPH, the Agency for Health care Research and Quality (AHRQ) via grant R01HS023317, United States Agency for International Development (USAID) under agreement number AID-OAA-A-15-00064, Global Obesity Prevention Center (GOPC) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the Office of the Director, National Institutes of Health (OD) under award number U54HD070725. It was also supported by NICHD via grant U01HD086861 and 5R01HD086013-02 and by National Institute of General Medical Sciences (NIGMS) via the Models of Infectious Disease Agent Study (MIDAS) network under grant 1 R01 GM127512-01A1. The funders did not have any role in the study design, collection, analysis and interpretation of data, writing the report, and the decision to submit the report for publication. The authors of this manuscript are responsible for its content, including data analysis. Statements in the manuscript do not necessarily represent the official views of, or imply endorsement by, National Institute of Health, AHRQ or HHS.
About CUNY SPH
The CUNY Graduate School of Public Health and Health Policy is committed to teaching, research, and service that creates a healthier New York City and helps promote equitable, efficient, and evidence-based solutions to pressing health problems facing cities around the world.
About PHICOR
Since 2007, PHICOR has been developing computational methods, models, and tools to help decision makers better understand and address complex systems in health and public health. Follow @PHICORTeam for updates.
Media Contact
Barbara Aaron
[email protected]
Original Source
https:/