Credit: Department of Nephrology,TMDU
Researchers from Tokyo Medical and Dental University (TMDU) find that immune system signaling molecule TNF-α may trigger high blood pressure in patients with chronic kidney disease
Tokyo, Japan – Detecting threats, sending out response molecules, and altering gene expression–our immune system works tirelessly day and night to protect us from invading pathogens and maintain general health and wellbeing. But in a study published this month in peer-reviewed journal Kidney International, a group of researchers from Tokyo Medical and Dental University (TMDU) in Japan have found a link between the immune system and high blood pressure in patients with chronic kidney disease (CKD).
CKD affects almost 800 million people worldwide and is the underlying cause of over a million deaths each year. One of the major complications of CKD is high blood pressure, or hypertension, and studies have shown that controlling blood pressure is an important factor in preventing CKD progression. However, many CKD patients display increased salt-sensitivity, a condition where blood pressure is unduly influenced by dietary salt intake, making it much harder to control.
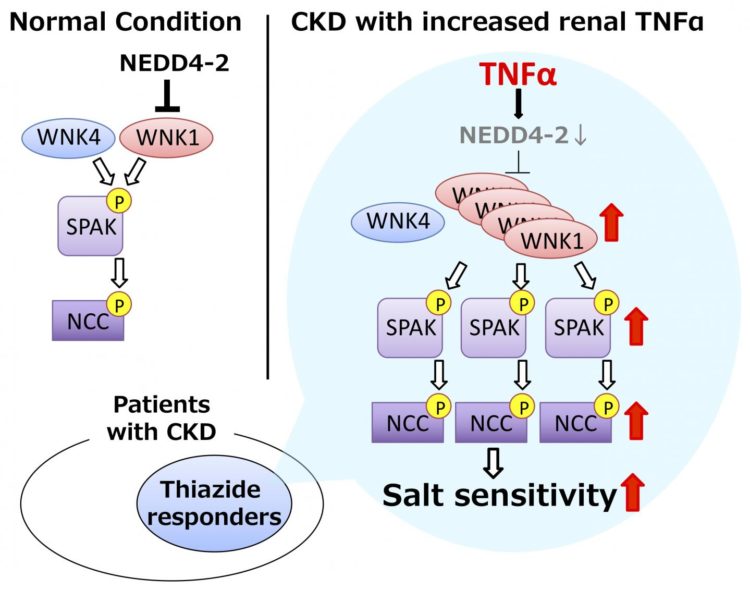
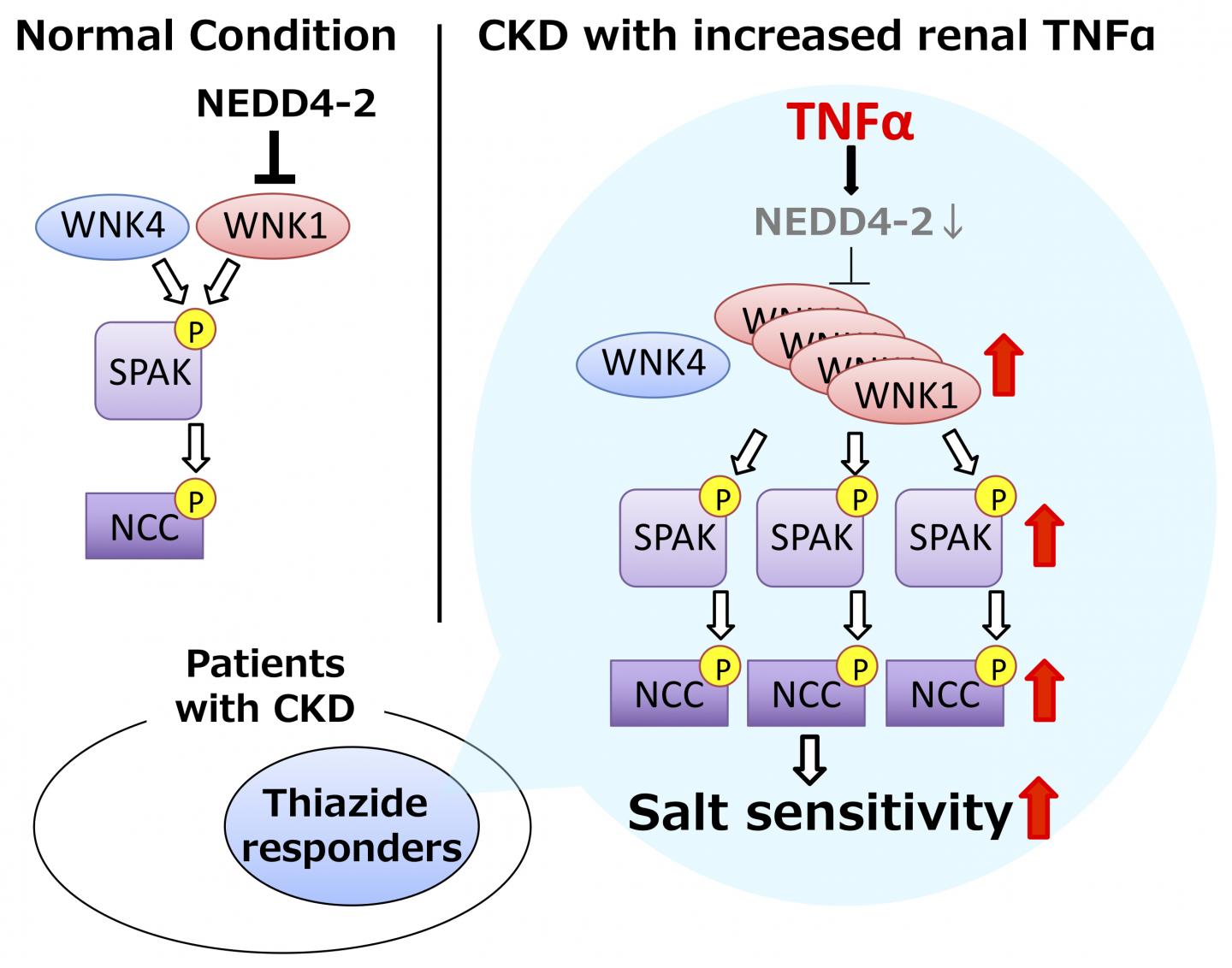
Inappropriate over-activation of a pathway called the WNK-SPAK-NCC phosphorylation cascade increases salt reabsorption in the kidney, leading to salt-sensitive hypertension. However, whether this pathway causes hypertension in CKD patients and what regulates the phosphorylation cascade had not been investigated.
Using a mouse model of disease, the researchers confirmed that mice with CKD had increased levels of the WNK1 protein in their kidneys, causing increased activation of the downstream proteins SPAK and NCC. When fed a high salt diet, the WNK-SPAK-NCC pathway remained activated in CKD mice, leading to salt-sensitive hypertension.
The researchers then looked to several recent studies suggesting that the immune system may play a role in salt sensitivity. Sure enough, levels of pro-inflammatory cytokine TNF-α were elevated in the kidneys of CKD mice, and provision of TNF-α resulted in increased levels of WNK1.
“Interestingly, TNF-α did not increase the transcription of WNK1, suggesting that it somehow prevented the degradation of mature WNK1 protein instead,” says corresponding author of the study Dr Eisei Sohara. “Based on this hypothesis, we confirmed that TNF-α enhances WNK1 protein levels by preventing the transcription of NEDD4-2 E3-ligase, a protein that normally degrades mature WNK1.” By inhibiting TNF-α, the researchers were able to reverse the salt sensitivity of CKD mice fed a high salt diet, confirming the link between the immune system and salt sensitivity.
Thiazide diuretics, NCC inhibitors, are widely used antihypertensive drugs, but their efficacy varies among patients with CKD. To achieve precision medicine, it is important to predict the efficacy of medication beforehand. Patients with enhanced activity of NCC are considered to respond well to thiazide diuretics. Therefore, finding of this study may contribute to better choice of antihypertensives in the future.
###
The article, “Renal TNFα activates the WNK phosphorylation cascade and contributes to salt-sensitive hypertension in chronic kidney disease,” was published in Kidney International at DOI: 10.1016/j.kint.2019.11.021.
Media Contact
Eisei SOHARA
[email protected]
Original Source
http://www.
Related Journal Article
http://dx.