Credit: RMIT University
Researchers have discovered an immune control switch that could protect the brains of premature babies, who often suffer brain injuries when their immune response goes into overdrive.
Through a series of clinical and pre-clinical studies, an international research team has for the first time worked out how to calm down hyperactive microglia, the brain’s immune cells.
The research points to a potential treatment for reducing brain injury in premature babies, showing microglia could be successfully targeted with drugs to control their harmful overactive behaviour.
The research, conducted over seven years by scientists and clinicians from Australia, France, the United Kingdom, Germany, Singapore and Sweden, is published in the journal Brain.
About 15 million babies are born prematurely around the world each year and rates of preterm birth are increasing in developed countries. In Australia, around 8% of babies are born prematurely (before 37 weeks gestation).
Premature birth is the most common cause of death and disability in children under 5 and up to 60% of babies born too early will have lifelong problems including attention-deficit disorders, autism, cerebral palsy and epilepsy.
Senior co-author, RMIT University’s Dr Bobbi Fleiss, said previous research had shown that exposure to inflammation was a driver of both premature birth and brain injury in babies.
“Inflammation is our body’s natural way of fighting infection, but the immune cells that drive this response can react too strongly in the developing brain and go into hyperdrive,” Fleiss, a Vice-Chancellor’s Research Fellow at RMIT, said.
“This intense immune response not only damages the baby’s brain, it diverts those cells from their other job of supervising brain development.
“We’ve discovered a way to tone down the hyperactivity without affecting the critical brain building work, using a microglia targeted therapeutic approach.
“It’s incredibly exciting because until now, we’ve known so little about the mechanisms that control the behaviour of microglia.
“This discovery gives us a solid way forward for developing new brain-protective therapies that will help millions of premature babies, and their families, around the world.”
Senior co-author, Professor Pierre Gressens from Inserm and the University of Paris, said doctors currently had no treatment options for stopping or preventing brain injury in premature babies.
“Inflammatory activation of microglia in the developing brain is associated with permanent neurological impacts in 9 million preterm babies around the globe every year,” Gressens said.
“There is a lot more work ahead to develop our treatment for clinical use, but these findings bring us significantly closer to delivering life-changing therapies for these vulnerable infants.”
Protecting white matter
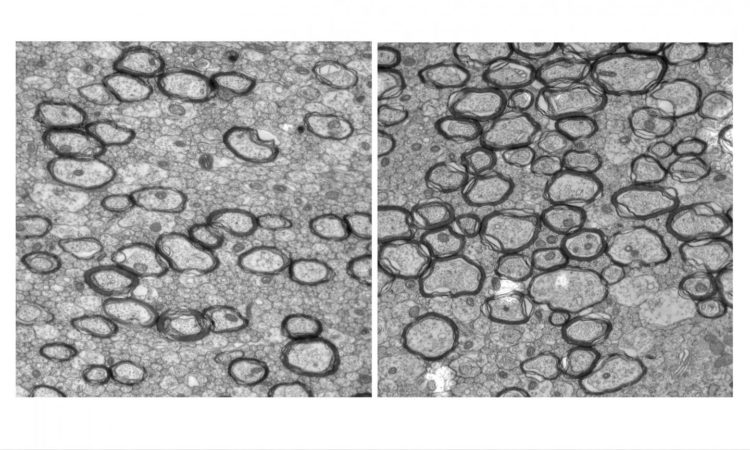
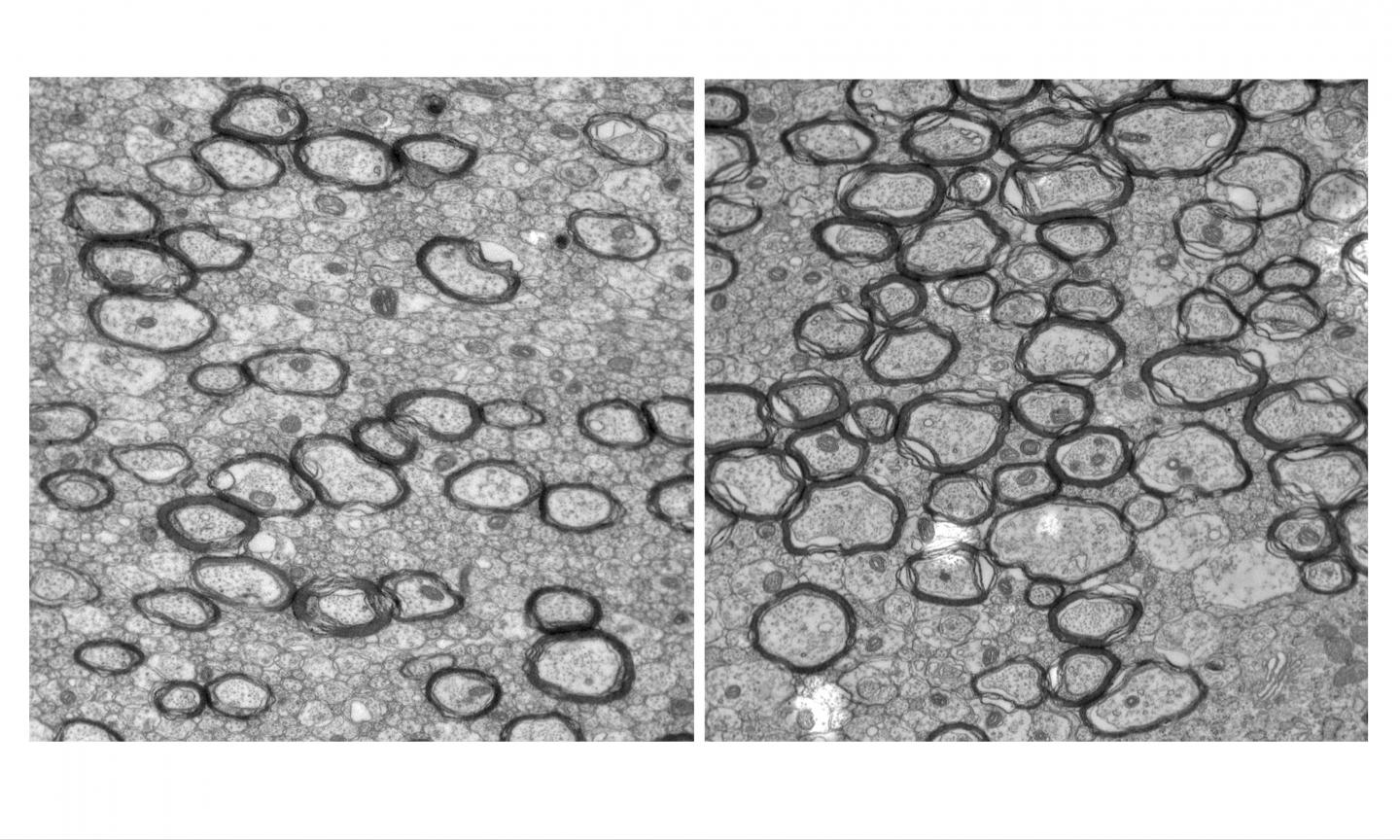
When microglia go into overdrive, they harm the brain’s white matter – a protective cocoon of fat that insulates nerve fibres and helps electrical signals move around the brain and body quickly and effectively.
If there is not enough white matter or if it is damaged, nerve pulses travel too slowly, affecting movement and cognition.
Pathway to treatment
The key to controlling the harmful behaviour of the microglia is a signalling pathway known as the Wnt.
In animal trials, researchers tested a drug that targets the Wnt pathway and keeps it active during inflammation.
The treatment prevented the microglia’s harmful hyperactivity, reducing damage to white matter as well as long-term memory problems associated with preterm birth.
Genetic differences
The research also revealed that in premature babies, genetic differences in the Wnt pathway are linked with different levels of brain connectivity and white matter structure.
This natural variance could in future be used for prognosis, to help doctors predict which premature babies may need extra support through their lives to overcome cognitive or physical problems.
Global collaboration
The collaboration involved clinicians and scientists from King’s College London, Institut Pasteur, Universite? Paris Descartes, PremUP, Pitie? Salpe?trie?re Hospital, Universite? Paris 13, Conservatoire National des arts et me?tiers, Guy’s and St Thomas’ NHS Foundation Trust, University of Edinburgh, Max Delbrueck Center for Molecular Medicine in the Helmholtz Society, Centre Hospitalier Sainte Anne, Duke-NUS Medical School and Gothenburg University.
The researchers acknowledge the support of Genisphere LLC (Hatfield PA, USA), developers of a DNA-based targeted drug delivery platform used in the trials. The novel 3DNA nanocarrier was shown to carry the drug through the body and precisely target the microglia.
RMIT has recently signed an agreement with Genisphere to further the research, with the aim of translating the findings into clinical therapies.
###
The research was funded in part by the Cerebral Palsy Alliance.
“Decreased microglial Wnt/β-catenin signalling drives microglial pro-inflammatory activation in the developing brain” is published in Brain (DOI: 10.1093/brain/awz319).
Media Contact
Gosia Kaszubska
[email protected]
61-417-510-735
Related Journal Article
http://dx.