The advancement, made possible by tiny photonic implants, could lead to new treatments for cancer, mental disorders
Credit: University at Buffalo
BUFFALO, N.Y. — It seems like everything is going wireless these days. That now includes efforts to reprogram the human genome.
A new University at Buffalo-led study describes how researchers wirelessly controlled FGFR1 — a gene that plays a key role in how humans grow from embryos to adults — in lab-grown brain tissue.
The ability to manipulate the gene, the study’s authors say, could lead to new cancer treatments, and ways to prevent and treat mental disorders such as schizophrenia.
The work — spearheaded by UB researchers Josep M. Jornet, Michal K. Stachowiak, Yongho Bae and Ewa K. Stachowiak — was reported in the June edition of the Proceedings of the Institute of Electrical and Electronics Engineers.
It represents a step forward toward genetic manipulation technology that could upend the treatment of cancer, as well as the prevention and treatment of schizophrenia and other neurological illnesses. It centers on the creation of a new subfield of research the study’s authors are calling “optogenomics,” or controlling the human genome through laser light and nanotechnology.
“The potential of optogenomic interfaces is enormous,” says co-author Josep M. Jornet, PhD, associate professor in the Department of Electrical Engineering in the UB School of Engineering and Applied Sciences. “It could drastically reduce the need for medicinal drugs and other therapies for certain illnesses. It could also change how humans interact with machines.”
From “optogenetics” to “optogenomics”
For the past 20 years, scientists have been combining optics and genetics — the field of optogenetics — with a goal of employing light to control how cells interact with each other.
By doing this, one could potentially develop new treatments for diseases by correcting the miscommunications that occur between cells. While promising, this research does not directly address malfunctions in genetic blueprints that guide human growth and underlie many diseases.
The new research begins to tackle this issue because FGFR1 — it stands for Fibroblast Growth Factor Receptor 1 — holds sway over roughly 4,500 other genes, about one-fifth of the human genome, as estimated by the Human Genome Project, says study co-author Michal K. Stachowiak.
“In some respects, it’s like a boss gene,” says Stachowiak, PhD, professor in the Department of Pathology and Anatomical Sciences in the Jacobs School of Medicine and Biomedical Sciences at UB. “By controlling FGFR1, one can theoretically prevent widespread gene dysregulations in schizophrenia or in breast cancer and other types of cancer.”
Light-activated toggle switches
The research team was able to manipulate FGFR1 by creating tiny photonic brain implants. These wireless devices include nano-lasers and nano-antennas and, in the future, nano-detectors.
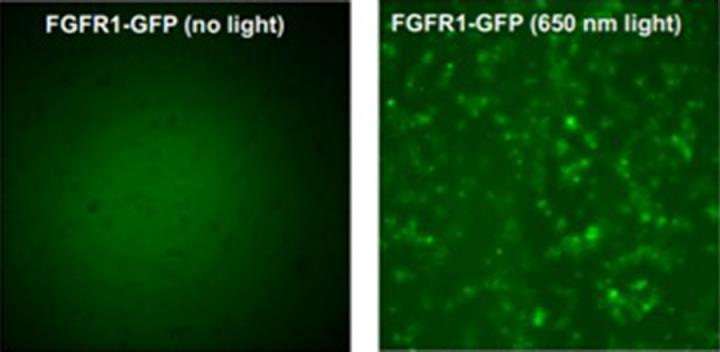
Researchers inserted the implants into the brain tissue, which was grown from induced pluripotent stem cells and enhanced with light-activated molecular toggle switches. They then triggered different laser lights — common blue laser, red laser and far-red laser — onto the tissue.
The interaction allowed researchers to activate and deactivate FGFR1 and its associated cellular functions — essentially hacking the gene. The work may eventually enable doctors to manipulate patients’ genomic structure, providing a way to prevent and correct gene abnormalities, says Stachowiak, who also holds an appointment in UB’s Department of Biomedical Engineering, a joint program between the Jacobs School and UB’s engineering school.
Next steps
The development is far from entering the doctor’s office or hospital, but the research team is excited about next steps, which include testing in 3D “mini-brains” and cancerous tissue.
Additional study authors include Pei Miao and Amit Sangwan of the UB Department of Electrical Engineering; Brandon Decker, Aesha Desai, Christopher Handelmann of the UB Department of Pathology and Anatomical Sciences; Liang Feng, PhD, of the University of Pennsylvania; and Anna Balcerak of the Maria Sklodowska-Curie Memorial Cancer Center and Institute of Oncology in Poland.
###
The work was supported by grants from the U.S. National Science Foundation.
Media Contact
Cory Nealon
[email protected]
Original Source
http://www.
Related Journal Article
http://dx.




