Crystallized drug prevents immune system rejection of transplanted pancreatic islet cells
Credit: Shady Farah
CAMBRIDGE, MA — When medical devices are implanted in the body, the immune system often attacks them, producing scar tissue around the device. This buildup of tissue, known as fibrosis, can interfere with the device’s function.
MIT researchers have now come up with a novel way to prevent fibrosis from occurring, by incorporating a crystallized immunosuppressant drug into devices. After implantation, the drug is slowly secreted to dampen the immune response in the area immediately surrounding the device.
“We developed a crystallized drug formulation that can target the key players involved in the implant rejection, suppressing them locally and allowing the device to function for more than a year,” says Shady Farah, an MIT and Boston Children’s Hospital postdoc and co-first author of the study, who is soon starting a new position as an assistant professor of the Wolfson Faculty of Chemical Engineering and the Russell Berrie Nanotechnology Institute at Technion-Israel Institute of Technology.
The researchers showed that these crystals could dramatically improve the performance of encapsulated islet cells, which they are developing as a possible treatment for patients with type 1 diabetes. Such crystals could also be applied to a variety of other implantable medical devices, such as pacemakers, stents, or sensors.
Former MIT postdoc Joshua Doloff, now an assistant professor of Biomedical and Materials Science Engineering and member of the Translational Tissue Engineering Center at Johns Hopkins University School of Medicine, is also a lead author of the paper, which appears in the June 24 issue of Nature Materials. Daniel Anderson, an associate professor in MIT’s Department of Chemical Engineering and a member of MIT’s Koch Institute for Integrative Cancer Research and Institute for Medical Engineering and Science (IMES), is the senior author of the paper.
Crystalline drug
Anderson’s lab is one of many research groups working on ways to encapsulate islet cells and transplant them into diabetic patients, in hopes that such cells could replace the patients’ nonfunctioning pancreatic cells and eliminate the need for daily insulin injections.
Fibrosis is a major obstacle to this approach, because scar tissue can block the islet cells’ access to the oxygen and nutrients. In a 2017 study, Anderson and his colleagues showed that systemic administration of a drug that blocks cell receptors for a protein called CSF-1 can prevent fibrosis by suppressing the immune response to implanted devices. This drug targets immune cells called macrophages, which are the primary cells responsible for initiating the inflammation that leads to fibrosis.
“That work was focused on identifying next-generation drug targets, namely which cell and cytokine players were essential for fibrotic response,” says Doloff, who was the lead author on that study, which also involved Farah. He adds, “After knowing what we had to target to block fibrosis, and screening drug candidates needed to do so, we still had to find a sophisticated way of achieving local delivery and release for as long as possible.”
In the new study, the researchers set out to find a way to load the drug directly into an implantable device, to avoid giving patients drugs that would suppress their entire immune system.
“If you have a small device implanted in your body, you don’t want to have your whole body exposed to drugs that are affecting the immune system, and that’s why we’ve been interested in creating ways to release drugs from the device itself,” Anderson says.
To achieve that, the researchers decided to try crystallizing the drugs and then incorporating them into the device. This allows the drug molecules to be very tightly packed, allowing the drug-releasing device to be miniaturized. Another advantage is that crystals take a long time to dissolve, allowing for long-term drug delivery. Not every drug can be easily crystallized, but the researchers found that the CSF-1 receptor inhibitor they were using can form crystals and that they could control the size and shape of the crystals, which determines how long it takes for the drug to break down once in the body.
“We showed that the drugs released very slowly and in a controlled fashion,” says Farah. “We took those crystals and put them in different types of devices and showed that with the help of those crystals, we can allow the medical device to be protected for a long time, allowing the device to keep functioning.”
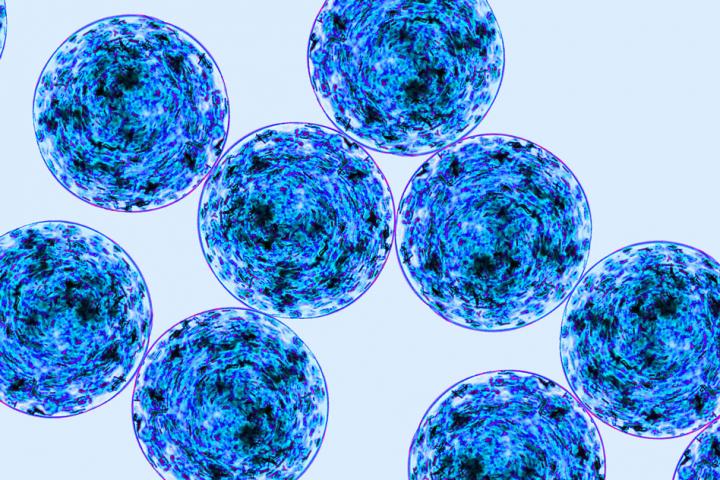
Encapsulated islet cells
To test whether these drug crystalline formulations could boost the effectiveness of encapsulated islet cells, the researchers incorporated the drug crystals into 0.5-millimeter-diameter spheres of alginate, which they used to encapsulate the cells. When these spheres were transplanted into the abdomen or under the skin of diabetic mice, they remained fibrosis-free for more than a year. During this time, the mice did not need any insulin injections, as the islet cells were able to control their blood sugar levels just as the pancreas normally would.
“In the past three-plus years, our team has published seven papers in Nature journals — this being the seventh — elucidating the mechanisms of biocompatibility,” says Robert Langer, the David H. Koch Institute Professor at MIT and an author of the paper. “These include an understanding of the key cells and receptors involved, optimal implant geometries and physical locations in the body, and now, in this paper, specific molecules that can confer biocompatibility. Taken together, we hope these papers will open the door to a new generation of biomedical implants to treat diabetes and other diseases.”
The researchers believe that it should be possible to create crystals that last longer than those they studied in these experiments, by altering the structure and composition of the drug crystals. Such formulations could also be used to prevent fibrosis of other types of implantable devices. In this study, the researchers showed that crystalline drug could be incorporated into PDMS, a polymer frequently used for medical devices, and could also be used to coat components of a glucose sensor and an electrical muscle stimulation device, which include materials such as plastic and metal.
“It wasn’t just useful for our islet cell therapy, but could also be useful to help get a number of different devices to work long-term,” Anderson says.
###
The research was funded by JDRF, the National Institutes of Health, the Leona M. and Harry B. Helmsley Charitable Trust Foundation, and the Tayebati Family Foundation.
Other authors of the paper include MIT Principal Research Scientist Peter Muller; MIT grad students Atieh Sadraei and Malia McAvoy; MIT research affiliate Hye Jung Han; former MIT postdoc Katy Olafson; MIT technical associate Keval Vyas; former MIT grad student Hok Hei Tam; MIT postdoc Piotr Kowalski; former MIT undergraduates Marissa Griffin and Ashley Meng; Jennifer Hollister-Locke and Gordon Weir of the Joslin Diabetes Center; Adam Graham of Harvard University; James McGarrigle and Jose Oberholzer of the University of Illinois at Chicago; and Dale Greiner of the University of Massachusetts Medical School.
Media Contact
Sarah McDonnell
[email protected]
Original Source
http://news.