Researchers from the Universities of Geneva and Franche-Comté have developed an innovative device that investigates a patient’s platelet capacity in near real-life conditions so that bleeding can be stopped (haemostasis)
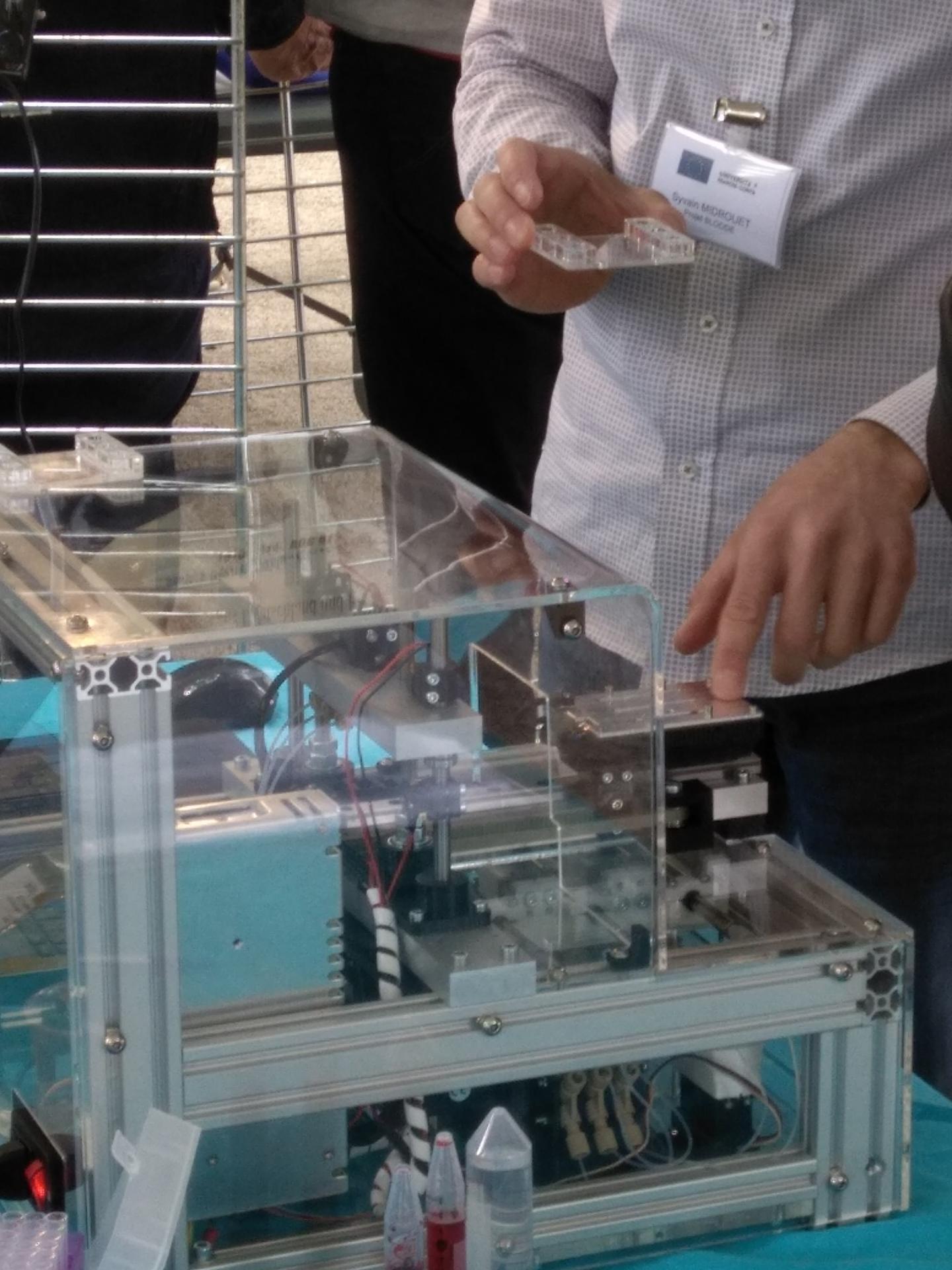
Credit: © Université de Franche-Comté
Various diseases can cause haemorrhages or thromboses, sometimes fatal, resulting in particular from complications during surgery. This may take the form of a dysfunction of the platelets (haemostasis), the blood cells the role of which is to plug the holes in the damaged blood vessels. Researchers from the University of Geneva (UNIGE), the University of Franche-Comté (UFC) and the Etablissement français du Sang (Bourgogne Franche Comté), have developed a device – known as BlooDe – in partnership with the University Hospitals of Geneva (HUG) and the CHU of Dijon and Besançon to study the plugging capacity of platelets. BlooDe can detect deficient platelet-related haemostasis of a subject effectively and in advance of an invasive procedure. It artificially reproduces blood circulation and holes in the vessel walls, and can test patient’s platelets with sufficient accuracy in under an hour using only a few millilitres of blood. These results are the fruit of a collaboration supported by the Interreg programme, which is the subject of a closing meeting on 26 June.
A failure of the haemostatic system – our ability to fight bleeding – can cause serious bleeding (when the blood doesn’t stop flowing) or thrombosis (when the blood no longer flows). In the most severe cases, this can result in the patient’s death or cause complications in her or his daily life with outbreaks of bleeding which, although not profuse, are uncomfortable. The blood platelets provide the first line of defence against bleeding by quickly plugging the holes in the walls of the blood vessels. Coagulation, as it is properly known, then follows and consolidates the wall; it is this process that is impaired in haemophilia.
It is possible to count the platelets to establish whether they are in sufficient numbers to perform this task. But there is still no good way of determining whether, even if there are enough of them, they are fulfilling their role correctly in the blood as it moves. “Knowing the haemostatic capacity of a patient is absolutely essential before a medical intervention involving a risk of haemorrhaging,” says Thomas Lecompte, a professor in UNIGE’s Faculty of Medicine and a doctor in the HUG Department of Medicine.
“A drug treatment can influence this ability either by slowing it down or increasing it, which leads to the risk of haemorrhage or thrombosis respectively. These dangers could be avoided if we knew more precisely how long is needed for the platelets to plug a hole. But we can’t carry out this exploration any more by making a small superficial cut in the skin in the forearm, as was the case for many years.”
Device that closely mimics the real conditions of circulating blood
The UNIGE and UFC Franche-Comté scientists joined forces to develop a device to analyse the work of each patient’s platelets at speed using funding provided by the Switzerland-France 2014-2020 Interreg programme amounting to 445’000 euros (European, federal and cantonal funds in Switzerland). “We needed to recreate a system that not only reproduced the movement of liquid blood but also the holes in the vessel walls,” explains Wilfrid Boireau, director of the Department of Micro Nano Sciences and Systems (MN2S) at the FEMTO-ST Institute (UFC – CNRS). When the blood leaves the vessel because of a breach, it encounters elements that were hidden while the vessel was intact (cells and tissues). “These encounters trigger the ‘alarm system’ that enables the platelets to intervene to plug the hole,” says the French researcher.
The scientists created a small device, known as BlooDe, that reproduces the movement of the circulating blood, and into which disposable cartridges are inserted. A pump system circulates the blood so that it can be analysed in micro-channels built inside the cartridges. “A few millilitres is all that is needed to obtain an informative result”, explains professor Lecompte. The blood then circulates in an artificial equivalent of the damaged vascular wall and the platelets come into play. “Then we need to see how long it takes the platelets to accumulate in this spot in sufficient quantities to stop the bleeding.” In an individual without a haemostatic disorder, five minutes is enough. “After 10 minutes, there is a real concern that needs to be factored in when treating the patient.”
BlooDe reliably mimics platelet functioning as closely as possible to what happens in the body (in vivo); it provides accurate data about the subject’s haemostatic capacity. “In less than an hour, we can have all the information needed to treat the patient properly,” adds professor Lecompte. In other words, BlooDe fulfils two main functions: in people suffering from a haemostatic system failure, it can be used to identify whether the failure comes from the malfunctioning of the platelets in their natural environment; and in individuals who are going to be operated on, it tests their haemostatic capacity so that the appropriate drug therapy if needed can be identified to minimize risks.
Pre-series of new prototype envisionned for 2021
The BlooDe prototype has successfully passed its very first laboratory tests. In order to consider large-scale clinical validation and commercialisation, the researchers are now working on upgrading some of its parts, including the cartridges, and are starting to scale up in preparation for industrial production. It is also currently being used under real medical conditions. «Our goal is to find an intermediary from an industry that specialises in in vivo devices in two years,» concludes professor Lecompte.
###
Media Contact
Thomas Lecompte
[email protected]




