The new technology is focused on improving detection and diagnosis of congenital heart disease in infants and children.
Credit: Image provided by the researchers
A new study by biomedical engineering researchers at the University of Arkansas could significantly improve methods for detecting and diagnosing congenital heart disease in infants and small children.
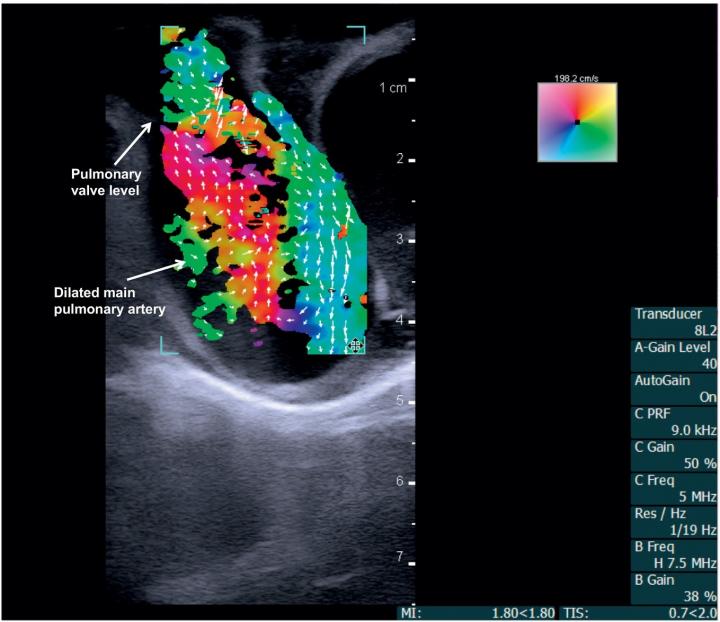
The researchers, collaborating with cardiologists at Arkansas Children’s Hospital in Little Rock, tested a new ultrasound technology called vector flow imaging for the first time on pediatric patients to create detailed images of the internal structure and blood flow of the babies’ hearts. The images can be still or moving, and can be taken from any angle.
“Vector flow imaging technology is not yet possible in adults, but we have demonstrated that it is feasible in pediatric patients,” said Morten Jensen, associate professor of biomedical engineering at the U of A. “Our group demonstrated that this commercially available technology can be used as a bedside imaging method, providing advanced detail of blood flow patterns within cardiac chambers, across valves and in the great arteries.”
Jensen performed the study with a multidisciplinary team, including Dr. Hanna Jensen, clinical assistant professor of biomedical engineering at the U of A; Dr. Thomas Collins, clinical associate professor of pediatric cardiology at Stanford University School of Medicine; and researchers at University of Arkansas for Medical Sciences (UAMS) and Cincinnati Children’s Hospital Medical Center. Their findings were published in Progress in Pediatric Cardiology.
Roughly 1 percent of all babies are born with some type of congenital heart defect. Fortunately, the majority of these defects will never have any significant impact as the child grows into adulthood and old age. Pediatric cardiologists detect and diagnose congenital heart disease through multiple processes, including echocardiography. This imaging method is based on ultrasound and assesses the overall health of the heart, including valves and muscle contraction.
Although ultrasound provides essential information about cardiac valve function in babies and small children, it has critical limitations. It cannot accurately obtain details of blood flow within the heart. This is due primarily to the inability to align the ultrasound beam with blood-flow direction.
Using a BK5000 Ultrasound machine with built-in vector flow imaging, the researchers performed successful tests on two pigs, one with normal cardiac anatomy and one with congenital heart disease due to a narrow pulmonary valve and a hole within the heart. The researchers then compared the vector flow images to direct examination of the pigs’ hearts.
The researchers subsequently used the imaging system to take cardiac images of two three-month-old babies, one with a healthy, structurally normal heart and one with congenital heart disease because of an abnormally narrow aorta. With both patients, the technology enabled total transthoracic imaging of tissue and blood flow at a depth of 6.5 centimeters. Abnormal flow and detailed cardiac anomalies were clearly observed in the patient with congenital heart disease.
All procedures, both animal and human, were performed at Arkansas Children’s Hospital with assistance from Dr. Elijah Bolin, pediatric cardiologist at UAMS.
“We are still getting used to having this great, new information readily available, and we’re excited about the future in both research and direct clinical advancements,” Bolin said.
“This technology will increase our ability to provide the best possible bedside diagnosis and greatly enhances our understanding of what is happening in hearts with complex abnormalities,” Stanford’s Collins said.
The researchers will perform additional studies to further quantify images using this recently developed technology.
###
This project was supported by the Arkansas Children’s Research Institute, the Collaborative Nutrition Pilot Grant and the Arkansas Research Alliance.
Jensen is an Arkansas Research Alliance Scholar.
Media Contact
Matt McGowan
[email protected]
Original Source
https:/




