Molecular process controls eye’s light-dependent vascular development
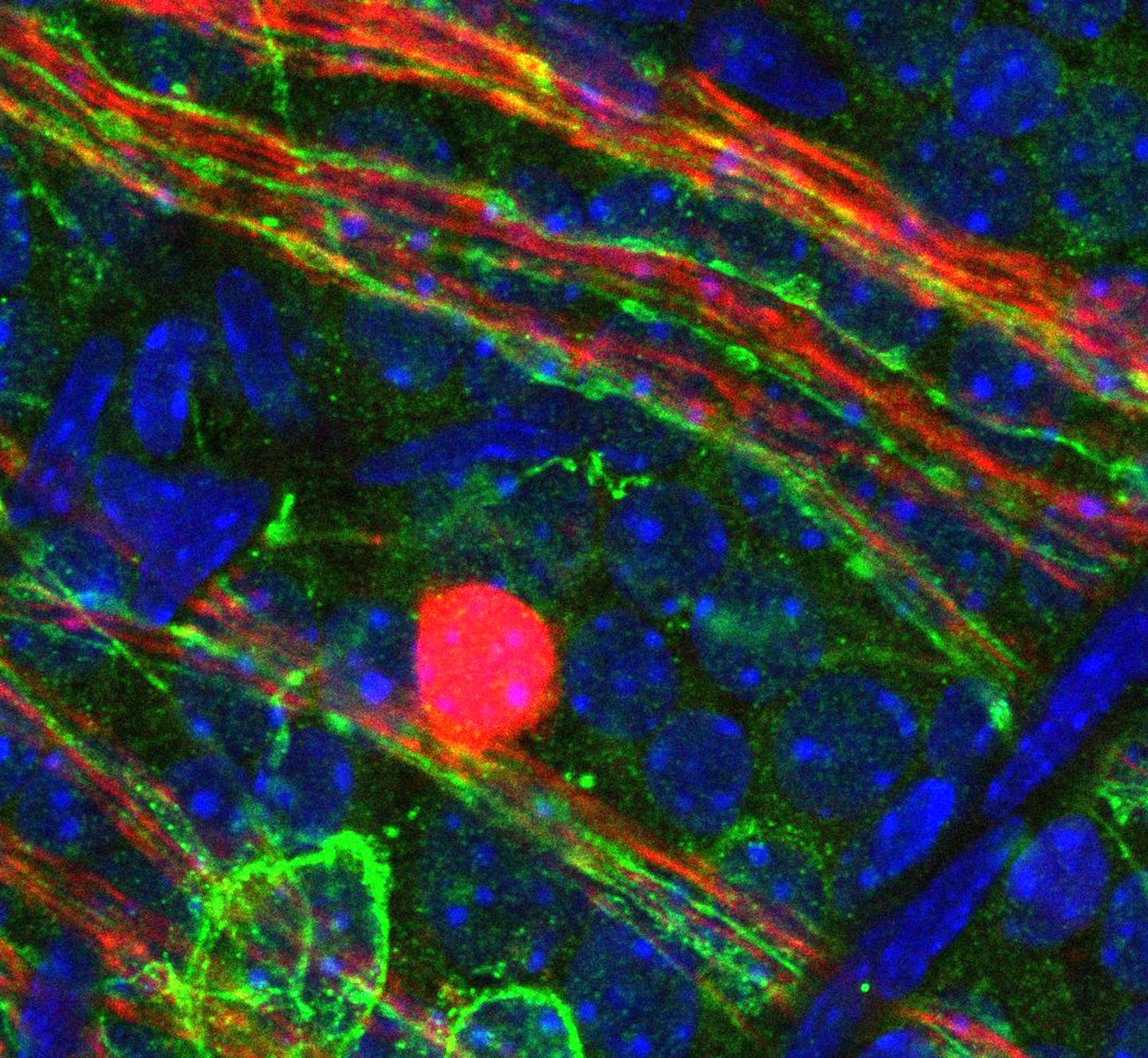
Credit: Cincinnati Children’s
CINCINNATI–Scientists discovered a light-dependent molecular pathway that regulates how blood vessels develop in the eye. The findings in Nature Cell Biology suggest it may be possible to use light therapy to help premature infants whose eyes are still developing avoid vision problems, according to researchers at Cincinnati Children’s Hospital Medical Center.
Called the opsin 5-dopamine pathway, the novel molecular process helps ensure blood-vessel development in the eye is appropriately balanced to prepare it for visual function. The process can be thrown out of balance in medically fragile premature babies. Researchers are looking for ways to prevent or treat the eye diseases retinopathy of prematurity and myopia (severe near-sightedness) that can result. Myopia is becoming a more common condition in adults around the globe.
“Our study indicates opsin 5-dopamine pathway is probably part of a light-dependent disease process for conditions like myopia, which is now a worldwide epidemic,” said Richard A. Lang, PhD, director of the Visual Systems Group at Cincinnati Children’s and study senior author. “It raises the interesting possibility that we might be able to use light exposure to treat conditions like retinopathy of prematurity after a premature infant is born or in people with myopia.”
The study is a collaboration of research institutions in the United States and Czech Republic led by Lang’s team in Cincinnati. The researchers used a variety of scientific methods to study eye development and the influences of the opsin 5-dopamine pathway in postnatal mice. Lang said opsin 5 is highly conserved in the chain of species evolution, enhancing the data’s potential relevance to humans.
Regression in Balance
During postnatal eye development in mice, an embryonic network of hyaloid blood vessels regresses in a process that requires precise timing in order for the mice to develop high-acuity vision.
The researchers demonstrate in their mouse models that the developing postnatal eye depends on light responses in the retina that are controlled by opsin 5, a protein that is expressed in special photoreceptor cells in the retina. Opsin 5 and the neurotransmitter dopamine–which promotes blood vessel regression–work in unison to regulate the eye’s balanced vascular development.
To show what would happen without the balancing influence of opsin 5, researchers studied genetically modified mice that do not express the OPN5 in the retina. Loss of opsin 5 increased levels of dopamine in the vitreous–the clear, gel-like substance in the eye. This caused hyaloid blood vessels in the still-developing eyes to regress very quickly, hindering normal eye development.
Shedding Light on the Problem
To test the influence of light stimulation, the researchers used 380 nanometer violet colored light to activate signaling via opsin 5. This reduced dopamine levels in the eye and produced other molecular changes that helped restore proper timing cues needed for appropriately balanced vascular development.
Previous studies have suggested that violet light and dopamine may be key regulators of eye development. And although findings in the current study require additional research to become clinically relevant to humans, the data do demonstrate that balanced coordination in the opsin 5-dopamine pathway is important to healthy eye development in baby mice, and possibly in human babies.
###
The study’s first author is Minh-Thanh T. Nguyen, PhD, until recently a research associate in the Lang laboratory. Collaborating institutions include: the University of Washington Medical School in Seattle; the Institute of Molecular Genetics and the Academy of Sciences of the Czech Republic; the Cleveland Clinic; the Emory University School of Medicine and the University of Cincinnati College of Medicine.
Funding support for the research came from: the National Institutes of Health (R01GM124246, R01EY026921, P30EY001730, R01 EY027077, R01 EY027711, R01 EY022917, R01EY004864, 2T32GM063483), funds from the Goldman Chair of the Abrahamson Pediatric Eye Institute at Cincinnati Children’s, a grant from BIOCEV-CZ.1.05/1.1.00/02.0109 (Z.K.). This work was supported by NIH grant 2T32GM063483, which supports the UCCOM/CCHMC Medical Scientist Training Program.
Media Contact
Nick Miller
[email protected]
Related Journal Article
http://dx.



