New findings have implications for heart failure, but also for cancer, diabetes and autoimmune disorders
A protein called mTOR receives information from these signals and then directs the cell to take action. And now, with data from cells and mice, researchers at Johns Hopkins Medicine…
view more
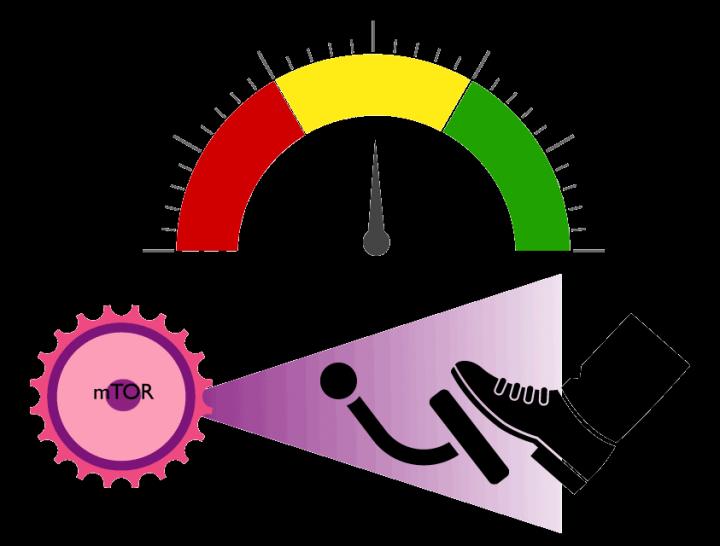
When normal cells grow, divide or do any job in the body, they do so in response to a whole slew of internal sensors that measure nutrients and energy supply, and environmental cues that inform what happens outside the cell. A protein called mTOR receives information from these signals and then directs the cell to take action. And now, with data from cells and mice, researchers at Johns Hopkins Medicine say they have uncovered a long-sought built-in molecular switch that behaves much like a car-brake–slowing mTOR’s action–and in this particular study prevents overworked hearts from enlarging.
The researchers report their findings on Jan. 30 in Nature, and say their discovery has potential implications for manipulating the molecular switch to treat not only heart disease–the focus of the current study–but also diabetes, kidney and lung disease, cancer and autoimmune disorders.
The protein mTOR, which stands for mechanistic target of rapamycin, has long been a focus of scientists because it is so important to normal cells yet also plays major roles in many diseases. It combines with other proteins to form a complex, the major one being known as mTORC1. Too much active mTORC1 is known to be bad for the heart and leads to damage and disease, and it is thought that controlling mTORC1 could effectively treat heart disease. Overworked hearts with too much active mTORC1 enlarge abnormally similar to body muscle that bulks up after lifting weights.
mTORs name derives from the immune-suppressant drug rapamycin, first extracted from Easter Island soil bacteria in the early 1970s, and later shown to block mTORC1 cold. The drug is prescribed to prevent transplanted organ rejection, and treat some rare cancers and genetic diseases.
But the complete shut-down of mTORC1 has its downside as it does so many things in normal cells, limiting prospects for using protein blockers as broader disease therapies, researchers say.
“The problem with the few drugs that we have to manipulate mTORC1 is that they are essentially turning it off, which also shuts down its normal function in the cells,” says senior study report author David Kass, M.D., the Abraham and Virginia Weiss Professor of Cardiology, professor of medicine, pharmacology and biomedical engineering at the Johns Hopkins University School of Medicine. “That means if you use it to, say, treat a tumor, you suppress the immune system as well, and might cause diabetes, or kidney and other organ damage by blocking mTORC1 in the other cells.”
Kass says researchers have spent decades in search of a simple switch to fine-tune mTORC1 activity – up and down – rather than making it be totally on or off, and he now has done it starting with a discovery with another protein of interest they had been studying for its role in heart disease.
Working in Kass’ laboratory, lead author and postdoctoral fellow Mark Ranek, Ph.D., was studying how this other protein called Protein Kinase G, protected heart tissue from damage and disease. He made the surprising discovery that turning on protein kinase G blocked mTORC1, and then figured out how this happens. The answer lies in a key regulator of mTORC1 called tuberin (dubbed TCS2 by researchers), which acts like an “antenna” for biochemical signals triggering or blocking cell growth, and regulating metabolism. Like the many other proteins known to alter tuberin, Ranek found protein kinase G altered tuberin by adding phosphates to it, but in a previously unidentified region that turned out to provide the sought after brake-like effect. Protein kinase G is also the target of drugs like sildenafil (commonly known as Viagra).
“Instead of turning mTORC1 off, we had something that looked more like a car brake, that was effective only if the car (mTORC1) was on and active,” says Ranek.
Using genetic engineering tools in heart muscle and connective tissue cells, the team mutated human tuberin protein in the specific places that were altered by protein kinase G. The alterations made the cells behave in one of two ways: one type of mutation “turned up” the effect of tuberin all the time while the other essentially “turned down” its effect all the time.
In the cells with tuberin “turned down”, nothing changed in the cells at rest. But, when the researchers treated the cells with hormones that encourage them to grow, mTORC1 was super-activated and the cells enlarged more than the cells with normal tuberin.
When the researchers looked at the cells that had tuberin “turned up”, they saw no changes in the cells when the same hormones were added.
Kass says the research team concluded that keeping tuberin “turned down” was like lifting the chemical foot off a brake pedal, triggering super-activity in mTORC1, while in the cells with tuberin “turned on”, the brake was pushed harder, and mTORC1 remained inactive despite the stimulating hormones.
To test the impact of the new tuberin mutations in living mice, the team used the same gene editing techniques to introduce the same types of tuberin mutations in the protein in all cells in live mice. The researchers then examined the hearts of mice with the mutant versions of tuberin compared to mice with normal tuberin.
Mice with tuberin “turned down” appeared normal and their hearts were the same as those in mice with normal tuberin. However, when the researchers increased the blood pressure that the heart had to work against, the hearts in the mutated mice grew much bigger on average twice as heavy and more than half the mice died over the next couple of weeks from heart failure. The researchers say that keeping tuberin “off” led to a hyper-activation of mTORC1 which they show caused the fatal damage.
Next, the researchers looked at hearts in mice that had tuberin “turned up”. Hearts from these mice also looked healthy, but when they were stressed using the same conditions of increased blood pressure, they remained healthy. The hearts were still normal in size and the mice stayed alive.
Mice, like humans have a pair of each chromosome in every cell. Kass and team reasoned that if both copies of the tuberin gene mutated to “turned up” resulted in normal hearts, what would happen if only one copy of the gene was mutated? In the next experiments, the researchers looked at what would happen if mice had only one copy of the gene mutation that made tuberin behave as if it always had phosphates attached. In those experiments the hearts stayed normal in size and had good function despite high blood pressure stress, showing just a single mutation was sufficient to protect the heart. On the flip side, they also found that only one copy of the mutation that “turned down” tuberin was all it took for larger hearts and early death to occur with pressure stress.
“We were struck by how potent the effect was, as only one copy of the gene mutation was needed to get the full protective effect,” says Ranek. “The benefit is that the new way to control mTORC1 by altering tuberin didn’t prevent its normal roles, but could keep mTORC1 in check from being turned on to too high of a level.”
“It was as if you are driving a car with one foot on the accelerator pedal and the other on the brake,” says Kass. “Here we found the brake control on the mTORC1 engine. Pushing it more slows it but doesn’t stop it completely, and lifting up on it speeds the car up,” adds Kass. “The bottom line is that by mutating tuberin to mimic protein kinase G’s effects, we slowed the engine, and mutating it so protein kinase G was ineffective, we cranked it up. But neither changed anything unless mTORC1 was stimulated, and only then did you find out whether the foot pressed the brake or released it.”
The authors caution that any clinical application of their findings to the heart probably won’t come by way of the genetic engineering of tuberin they performed in the lab.
“This would require some type of gene therapy, which means putting the gene into a virus that then transfers it to the heart,” says Kass. “However, the tuberin gene is too big to fit into viruses we currently have for this job.”
But drugs that activate protein kinase G, such as nitroglycerin and sildenafil, are currently used to relax arteries in patients with coronary heart disease, pulmonary hypertension, and erectile dysfunction, and they are already being actively explored for congestive heart failure. The new study shows how they may be particularly useful in heart diseases in which mTORC1 is too active.
“This is an important finding because it reveals a novel strategy that could be employed in future potential therapeutic efforts to protect the heart from damaging stress such as high blood pressure,” said Bishow Adhikari, Ph.D., a program officer for the study and a scientist with the National Heart, Lung, and Blood Institute, part of the National Institutes of Health, which helped fund the study.
There are other conditions, however, where altering the tuberin gene may be easier to accomplish. In particular, he says, because mTORC1 also plays a critical role in immune cell activation and memory, and these cells are now being genetically modified for cancer therapy, the discovery of the new control brake may eventually enhance the effectiveness of cancer immunotherapy treatments.
Because of the promise, several authors have formed a company to pursue further development of immune system controllers.
###
WATCH: Shrinking Diseased Hearts by Putting the Brakes on a Master Growth Controller
Hyperlink: https:/
Additional authors include Kristen Kokkonen-Simon, Anna Chen, Brittany Dunkerly-Eyring, Miguel Pinilla Vera, Christian Oeing, Chirag Patel, Taishi Nakamura, Guangshuo Zhu, Djahida Bedja, Masayuki Sasaki and Dong Ik Lee of Johns Hopkins with Jonathan Powell from the Bloomberg~Kimmel Institute for Cancer Immunotherapy in the Sidney-Kimmel Comprehensive Cancer Research Center; and Ronald Holewinski and Jennifer Van Eyk of Cedars Sinai Medical Center.
The research was supported by was supported by the National Heart Lung and Blood Institute (HL-135827, HL-119012, HL089297, T32-HL-07227, HHSN268201000032C, F31-HL134196 and F31-HL143905), the National Institute of Allergy and Infectious Diseases (R01AI077610 and R01AI091481), American Heart Association Post-Doctoral Fellowships, Deutsche Forschungsgemeinschaft OE 688/1-1, Fondation Leducq TransAtlantic Network of Excellence, Abraham and Virginia Weiss Professorship, Erika J. Glazer Endowed Chair in Women’s Heart Health, Barbra Streisand Women’s Heart Center and the Bloomberg~Kimmel Institute for Cancer Immunotherapy.
COI: Kass, Powell and Ranek are founders of and hold equity in Meta-T Cellular. Meta-T Cellular intends to license and further develop technology discussed in this publication that relates to the use of TSC2 modifications for immunological applications. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies.
Media Contact
Vanessa McMains
[email protected]
410-502-9410
Original Source
https:/




