Serendipitous observation opens the door for a precision medicine treatment
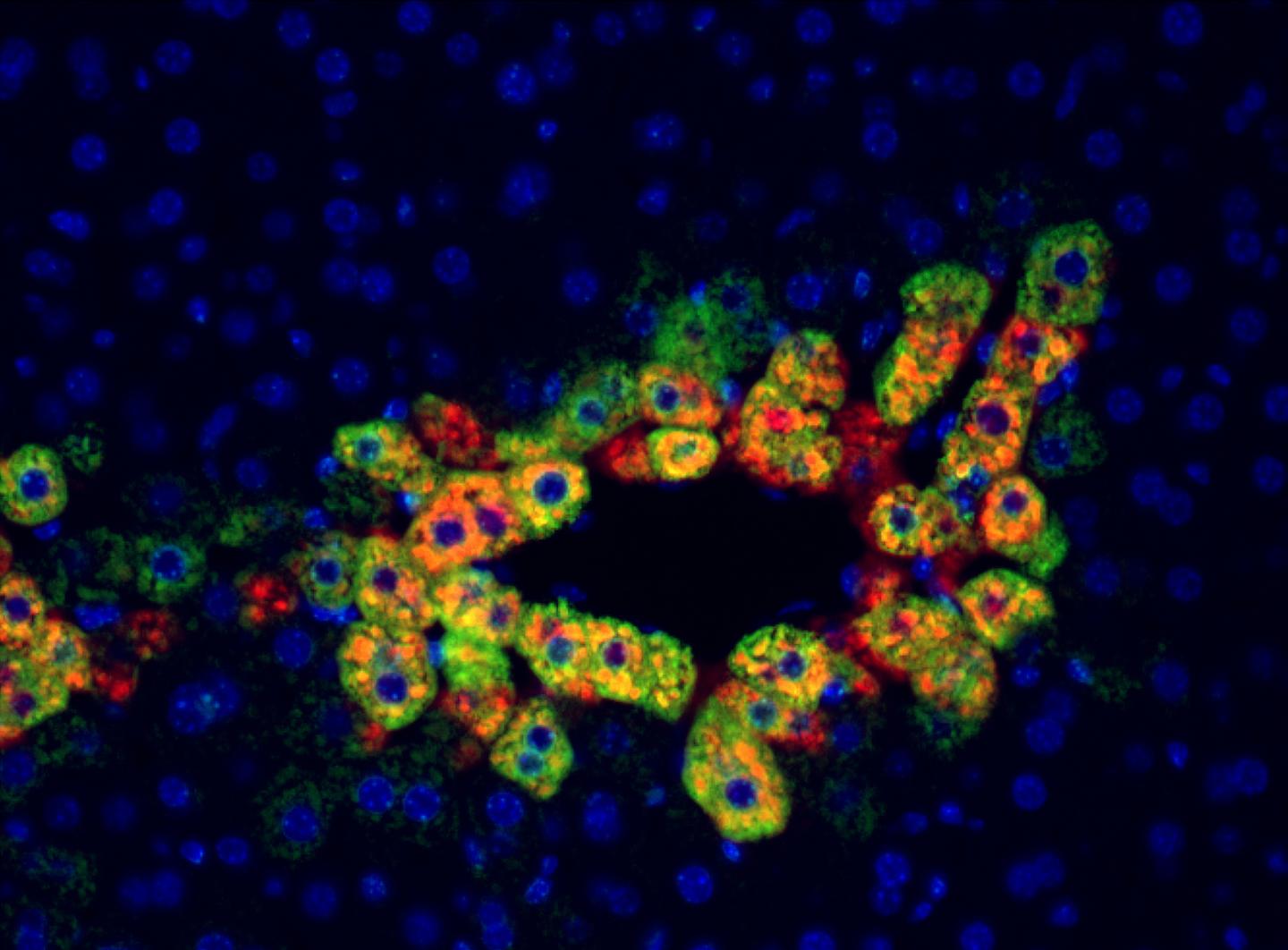
Credit: Cell Reports/University of Pittsburgh
Research from the University of Pittsburgh School of Medicine in animal models and patient tissues has identified a new molecular pathway in the liver that suggests a commonly used anti-rejection medication could be repurposed to treat certain liver cancers.
“What we’ve found is that liver cancers with a specific mutation in the β-catenin gene are possibly more susceptible to rapamycin, a commonly used anti-rejection medication in transplantation,” said Satdarshan Monga, M.D., professor of pathology and the founding director of the Pittsburgh Liver Research Center at Pitt’s School of Medicine and senior author of the study published in Cell Metabolism. “We think this gives us a new precision medicine approach to develop therapies for liver cancer, which often are very resistant to treatment.”
The current study began when Monga and his team made a serendipitous observation that a ring of cells surrounding the central vein, a blood vessel found within the liver, showed high levels of a protein called mTOR. The active mTOR protein, a nutrition and energy sensor central to cellular metabolism, was found in the same cells where β-catenin was known to be active.
Approximately 20 to 35 percent of liver cancers have a β-catenin mutation, but there is little understanding of how and why these mutations could be aiding the growth of cancerous cells. So, when Monga found similarly high levels of active mTOR in β-catenin mutated liver cancers, he wondered whether the two proteins could be functionally linked.
To trace the source of mTOR activation, the scientists created a mouse model of liver cancer in which they genetically mutated β-catenin, along with another gene called Met, specifically in liver cells. These mice developed liver cancers that were genetically very similar to those seen in humans.
Starting with increased mTOR activation, they followed the molecular breadcrumbs in these mice to show that β-catenin activated mTOR through an intermediate enzyme called glutamine synthase (GS). This molecular pathway was linked to energy intake, as fast-growing cancer cells, which consume more energy than normal cells, showed higher activity of GS and mTOR.
“I like to say these tumors are mTOR addicted,” said Monga, who also is an investigator at the McGowan Institute of Regenerative Medicine and the UPMC Hillman Cancer Center. “Activating mTOR kicks up the protein-making factories in these cells, giving them the resources to divide and grow.”
When the genetically modified mice were fed rapamycin – an immunosuppressant that inhibits mTOR – the tumors decreased in size, and when they added another drug that inhibited Met, the tumors were almost completely killed, showing that mTOR played an important role in helping these tumors grow.
The researchers note that a previous clinical trial in patients with liver cancer did not find a significant benefit for rapamycin, but the new findings suggest that perhaps if the pool were limited to patients with β-catenin mutations and mTOR-addicted tumors, the treatment would have been more successful.
“Current liver cancer therapies increase the likelihood of survival only by 3 or 4 months, so taking a precision medicine approach to identify the right patient could allow us to repurpose existing drugs to improve treatment success,” Monga said.
Beyond treating liver cancer, the study also points to ways in which we could reduce the risk of cancer recurrence in some patients undergoing liver transplant.
“While transplant patients are prescribed either rapamycin or a different immunosuppressant, those that have β-catenin mutated and mTOR-addicted tumors might benefit from using rapamycin as the preferred anti-rejection medication. We hope to conduct clinical trials in the near future to test rapamycin both in treating liver cancer and to prevent its recurrence in patients receiving liver transplants,” Monga said.
A complete listing of all the study authors can be found in the online article.
###
The study was funded by National Institutes of Health grants 1R01DK62277, 1R01DK100287, 1R01DK116993, T32CA186873, R01CA204586, and the German Research Foundation, DFG through SFB 974.
Monga received grant funding and served as a consultant to Abbvie and Dicerna but did not have any competing financial interests directly relevant to the current study.
About the University of Pittsburgh School of Medicine
As one of the nation’s leading academic centers for biomedical research, the University of Pittsburgh School of Medicine integrates advanced technology with basic science across a broad range of disciplines in a continuous quest to harness the power of new knowledge and improve the human condition. Driven mainly by the School of Medicine and its affiliates, Pitt has ranked among the top 10 recipients of funding from the National Institutes of Health since 1998. In rankings recently released by the National Science Foundation, Pitt ranked fifth among all American universities in total federal science and engineering research and development support.
Likewise, the School of Medicine is equally committed to advancing the quality and strength of its medical and graduate education programs, for which it is recognized as an innovative leader, and to training highly skilled, compassionate clinicians and creative scientists well-equipped to engage in world-class research. The School of Medicine is the academic partner of UPMC, which has collaborated with the University to raise the standard of medical excellence in Pittsburgh and to position health care as a driving force behind the region’s economy. For more information about the School of Medicine, see http://www.
http://www.
Media Contact
Arvind Suresh
[email protected]
412-509-8207
Related Journal Article
http://dx.




