Breast cancer survivors reported improvements in depression, pain, anxiety and sleep after self-administered acupressure
Credit: University of Michigan Rogel Cancer Center
ANN ARBOR, Michigan — A new study finds acupressure could be a low-cost, at-home solution to a suite of persistent side effects that linger after breast cancer treatment ends.
Researchers from the University of Michigan Rogel Cancer Center reported in 2016 that acupressure helped reduce fatigue in breast cancer survivors.
In the new study, they looked at the impact of acupressure on symptoms that frequently accompany fatigue in this population: chronic pain, anxiety, depression and poor sleep. They found acupressure improved all of these symptoms compared with standard care.
In the study, breast cancer survivors who reported fatigue were randomized to one of two types of acupressure or to usual care, which included typical sleep-management techniques. The women were taught how to find and stimulate the acupressure points so that they could perform it at home once per day for six weeks.
Of the 424 survivors experiencing fatigue from the original study, researchers found half had at least one other symptom and 17 percent experienced all of them.
“It was actually unusual for a woman to have just fatigue. These long-term side effects are a big problem. For some women, they are significant barriers in their life,” says study author Suzanna M. Zick, N.D., MPH, research associate professor of family medicine at Michigan Medicine.
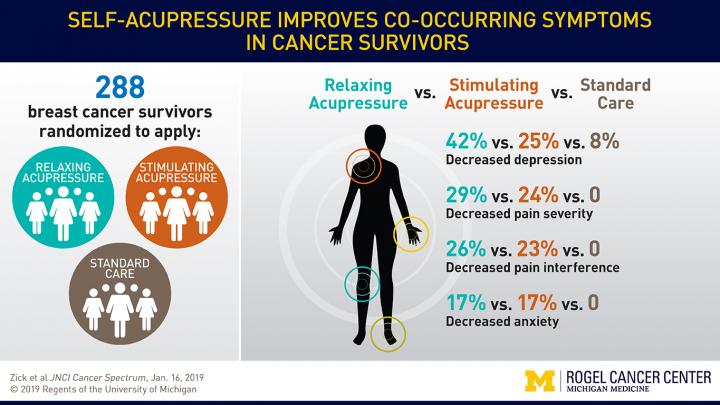
The new analysis focused on the 288 patients who reported symptoms in addition to fatigue. They were asked weekly about fatigue, sleep quality, depressive symptoms, anxiety and pain. Results are published in JNCI Cancer Spectrum.
Acupressure is derived from traditional Chinese medicine. It involves applying pressure with fingers, thumbs or a device to specific points on the body. Researchers tested two types of acupressure: relaxing acupressure, which is traditionally used to treat insomnia, and stimulating acupressure, which is used to increase energy. The two techniques differ by which points on the body are stimulated.
After six weeks, relaxing acupressure was significantly better than stimulating acupressure or standard care at improving depressive symptoms and sleep. Both types of acupressure were more effective than standard care for improving anxiety, severity of pain and pain interfering with daily life.
“If you have a person who is fatigued and depressed, it would be the obvious conclusion to use relaxing acupressure. For anxiety or pain, either approach might work,” Zick says.
The researchers also assessed whether improving one symptom helped improve other symptoms. They found that improving symptoms of depression improved sleep quality, accounting for about 20 percent of the improvement in fatigue.
“That means we don’t know 80 percent of what’s impacting fatigue. Depressive symptoms and sleep quality are a small part, and it makes sense. But clearly, there are other factors,” Zick says.
She suspects these symptoms impact several different mechanistic pathways, possibly impacting the brain in multiple ways. This means treatments will likely need to be tailored and varied based on a woman’s symptoms and other factors.
The researchers plan to gather more information using neuroimaging to understand the brain pathways involved. They’re also currently conducting two clinical trials to look at using an acupressure app. Working with U-M College of Engineering experts, they developed a special wand to assist patients in performing acupressure. The wand helps ensure appropriate pressure and tracks how long patients use it.
Acupressure is an appealing option because it can be done at home with minimal negative effects. The study showed that women could learn to apply correct pressure to the appropriate points. Some women reported minor bruising at the acupressure sites.
###
Additional authors: Ananda Sen, Afton L. Hassett, Andrew Schrepf, Gwen Karilyn Wyatt, Susan Lynn Murphy, John Todd Arnedt, Richard Edmund Harris
Funding: National Institutes of Health grants R01 CA151445 and 2UL1 TR000433-06
Disclosure: None
Reference: JNCI Cancer Spectrum, doi: 10.1093/jncics/pky064, published online Jan. 16, 2019
Resources:
University of Michigan Rogel Cancer Center, http://www.
Michigan Health Lab, http://www.
Michigan Medicine Cancer AnswerLine, 800-865-1125
Media Contact
Nicole Fawcett
[email protected]
734-764-2220
Original Source
https:/
Related Journal Article
http://dx.




