New Haven, Conn. — For many, the threat of the COVID-19 pandemic seems over. However, for patients whose immune systems are compromised by cancer or by cancer therapies, fear of COVID-19 infection and severe disease remains very real.
Credit: Image courtesy of Kontopoulou et al.
New Haven, Conn. — For many, the threat of the COVID-19 pandemic seems over. However, for patients whose immune systems are compromised by cancer or by cancer therapies, fear of COVID-19 infection and severe disease remains very real.
Currently, CDC guidance recommends that immunocompromised patients receive COVID-19 booster shots “as needed.” While this flexibility is useful for patients with complex medical conditions, more specific guidance is lacking as to when additional COVID-19 boosting would be most effective.
New research led by scientists at Yale University and the University of North Carolina at Charlotte provides this critically needed information. The rate at which additional COVID-19 boosters are needed for cancer patients, the researchers say, depends on the treatment they are receiving.
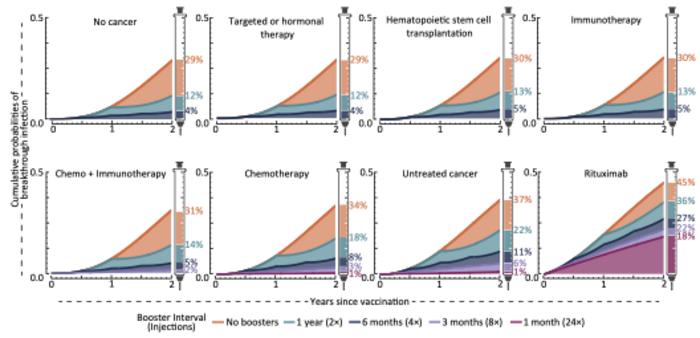
The study, published Aug. 21 in the Journal of the National Cancer Institute, quantifies the long-term likelihood of future infection among cancer patients undergoing various common therapies after they received updated Pfizer vaccine booster shots.
According to the research, increased boosting among cancer patients provides benefits similar to those obtained by non-cancer patients. The study predicts that one out of every three people who forgo boosting will be infected within two years. In contrast, boosting every six months reduces that risk to 1 in 20.
“It turns out that most cancer patients are protected nearly as well as the non-cancer population by COVID-19 boosting,” said Yale School of Public Health Professor Jeffrey Townsend, the study’s lead author. “But there is a big exception.”
“Some cancer therapies directly attack immune cells,” said the study’s co-leader Alex Dornburg, an assistant professor at the University of North Carolina at Charlotte. “This is great for battling blood cancers such as some lymphomas, but the death of immune cells also opens a window not only for COVID-19 infection, but for severe infection.”
For those cancer patients whose therapies directly impact the immune response, a much higher frequency of boosting could be very beneficial, the researchers said. With annual boosting, one out of every three patients on these therapies would still be vulnerable to contracting COVID-19 within two years without other interventions. Boosting every three months cuts this risk almost in half, the study said.
The researchers’ data-driven model of infection risks over time takes advantage of the large number of immunological studies of SARS-CoV-2 (the virus that causes COVID-19) and other coronaviruses. The extensive data available enabled them to assess the long-term risks of infection at a range of frequencies of boosting.
“These results are based on a typical patient with a typical immune response receiving common therapies,” said Townsend. “It remains the case that every patient may have mitigating factors that doctors must consider when advising whether and when an additional COVID-19 booster schedule may be appropriate.”
“Fears of severe COVID-19 are not restricted to cancer patients.” added Dornburg. “We hope to develop similar analyses that provide guidance to protect other patients who are especially vulnerable.”
Funding for the research was provided by the National Science Foundation.
Journal
JNCI Journal of the National Cancer Institute
DOI
10.1093/jnci/djad158
Article Title
Infection with alternate frequencies of SARS-CoV-2 vaccine boosting for patients undergoing antineoplastic cancer treatments
Article Publication Date
21-Aug-2023



