Updated guidelines published in Wilderness & Environmental Medicine provide most up-to-date and relevant clinical information to frontline providers in wilderness or austere environments incl new guidelines on diabetes management & spinal immobilization
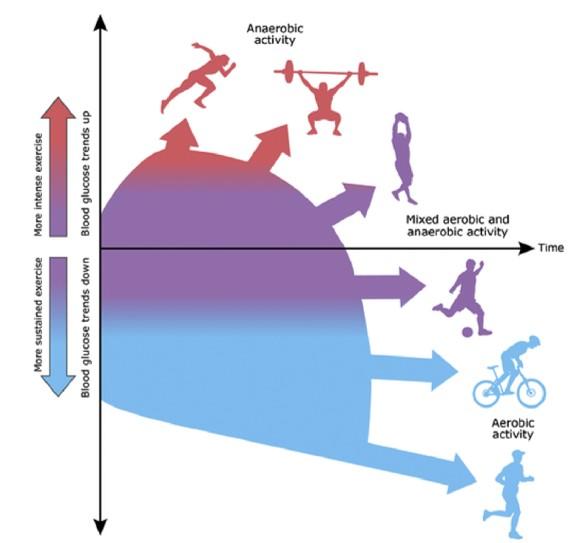
Credit: Illustration by Anne Greene, Senior Medical Illustrator, reproduced with permission from UpToDate, Inc. Copyright © 2017 Duration and intensity. Reproduced with permission from: Riddell MC. Management of exercise for children…
Philadelphia, February 5, 2020 – The Wilderness Medical Society (WMS) has released new clinical practice guidelines in a supplement to Wilderness & Environmental Medicine, published by Elsevier. This issue features updates to previously published clinical practice guidelines and newly developed guidelines on diabetes management and spinal immobilization in the wilderness setting.
These revised and new WMS clinical practice guidelines have been developed and guest-edited by Christopher Davis, MD, Department of Emergency Medicine-Wilderness and Environmental Medicine, University of Colorado School of Medicine, Aurora, CO, USA; Michael Caudell, MD, Department of Emergency Medicine, Medical College of Georgia at Augusta University, Augusta, GA, USA; and Tracy Cushing, MD, MPH, Department of Emergency Medicine, University of Colorado Hospital, Aurora, CO, USA. All recommendations are graded based upon the clinical strength of available evidence as outlined by the American College of Chest Physicians (ACCP).
“Clinical practice guidelines are increasingly necessary to help clinicians navigate and synthesize the expanding volume of available medical literature,” explained Dr. Davis. “Our guidelines are continuously updated to reflect the most current literature and recommendations for wilderness medicine pathology and are uniquely interdisciplinary in their authorship. Our goal is to provide the most up-to-date and relevant clinical information to frontline providers in wilderness or austere environments.”
“The WMS is committed to ensuring that each clinical practice guideline is developed by a working group representative of the best experts in the field and multidisciplinary in scope,” added Dr. Davis. “As an interdisciplinary author group, the impact of these guidelines is far reaching both in terms of scope of practitioners and in breadth of information. These address unique pathology such as altitude illness that are not covered in other medical literature and sometimes provide the ONLY clinical practice guidelines for particular illnesses.”
New clinical practice guidelines include:
Clinical practice guidelines for diabetes management
Athletes with both type 1 and type 2 diabetes are undertaking ever-expanding wilderness challenges. At least three individuals with diabetes have successfully reached the summit of Mount Everest. In a recent survey, people who self-identified as having diabetes represented seven percent of 3,000 surveyed ultramarathon runners. Both high and low blood sugar can be catastrophic in environments where there are limited resources, and glycemic control is more challenging in extreme conditions, needing additional monitoring, treatment adjustments, and careful planning beforehand.
The authors of a new guideline on diabetes management point out that there are so many variables that it is impossible to come up with a single set of guidelines. They recommend personalizing the medical care of each individual based on personal history and input, and advise adjusting insulin doses and diet plans according to the type and degree of activity that will be performed; an individual’s baseline level of fitness; the individual’s athletic and disease history; and the environment to which the athlete will be exposed. They also recommend that athletes with diabetes should carry a basic written plan developed with their endocrinologist describing their usual treatment regimen; a plan for basic adjustments in the back country; basics of hypo-/hyperglycemia management; and an emergency action plan.
Clinical practice guidelines for spinal cord protection
The low volume and quality of scientific evidence available does not support the current rationale for immobilizing a potential spine injury in the wilderness environment, according to the updated guideline on spinal injury care, suggesting that historic principles of out-of-hospital spinal injury care may have been more influenced by medicolegal implications and untested theory than by clinical or scientific evidence. The focus of this current guideline is to present an evidence-based approach to out-of-hospital care of an existing or potential spinal cord injury in wilderness environments that minimizes the possibility of neurologic deterioration or making the injury worse from the time of extrication to arrival at a medical facility. Current evidence suggests that rigid immobilization via collar or backboard can result in a worse patient outcome in both blunt and penetrating trauma. Instead, the guidelines propose that spinal motion restriction (SMR) may be the most appropriate mechanism currently available.
Other updated guidelines cover the prevention and treatment of acute altitude illness; prevention and treatment of frostbite; prevention and treatment of heat illness; prevention and treatment of drowning; water disinfection for wilderness, international travel, and austere conditions; and out-of-hospital evaluation and treatment of accidental hypothermia. They also highlight several important questions that remain to be addressed and could serve as a focus for future research, such as, the role of acetazolamide in preventing and treating high altitude cerebral edema; determining the optimal rate of ascent to prevent altitude illness; the role of staged ascent, preacclimatization, and hypoxic tents in altitude illness prevention; optimal methods of resuscitating hypothermic patients in cardiac arrest; and the use of technological innovations to allow access to wilderness pursuits such as big wall rock climbing and scuba diving that have historically been off limits to those with diabetes.
Dr. Cushing added a note of caution about the challenges faced in developing guidelines for illnesses encountered in the wilderness. “Wilderness recreation is increasingly popular. Accordingly, more individuals are at risk today than ever before. However, it is challenging to design and execute randomized clinical trials, as the illnesses we treat are not only rare, they also occur in challenging and remote environments.”
“Previously published guidelines have been some of the most highly-cited articles in Wilderness & Environmental Medicine. It is our foremost goal to continue the tradition of bringing forward the best available data to the wilderness medical provider,” concluded the guest editors.
###
Media Contact
Theresa Monturano
[email protected]
215-239-3711
Original Source
https:/




