A nationwide population-based study conducted by researchers at Shinshu University in Japan has unveiled significant variations in the incidence and risk of colorectal cancer (CRC) among patients diagnosed with different subtypes of steatotic liver disease (SLD). This groundbreaking research not only highlights the health implications associated with SLD but also underscores the critical need for tailored screening efforts in different patient populations. SLD encompasses a heterogenous class of liver diseases, including metabolic dysfunction-associated SLD (MASLD), MASLD with increased alcohol intake (MetALD), and alcohol-associated liver disease (ALD).
Recent epidemiological studies have recognized both alcoholic and non-alcoholic fatty liver diseases as substantial risk factors for colorectal cancer. Notably, non-alcoholic fatty liver disease has gained attention as a prevalent condition affecting more than a quarter of the global population, often correlated with metabolic disorders such as diabetes and obesity. The intricacies of SLD, however, have not been fully explored concerning their role as precursors to CRC, prompting the urgency for research that delineates these relationships.
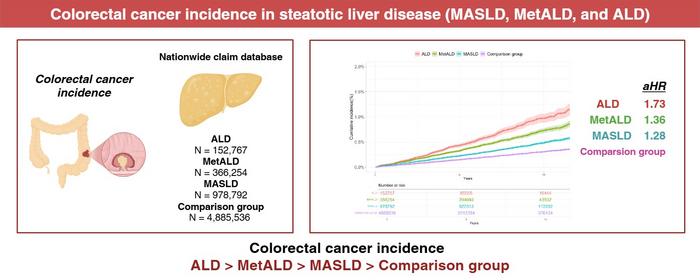
For this recent study, Dr. Takefumi Kimura and his interdisciplinary team employed a robust methodology to compare the risk factors associated with CRC across various subgroups of patients with SLD. By analyzing data from approximately 6.38 million individuals, they reinforced the hypothesis that the interplay between metabolic dysfunction and alcohol consumption significantly influences CRC risks. Their findings indicated that individuals with alcoholic liver disease exhibited a 1.73-fold increased risk of developing colorectal cancer compared to those without liver issues, which is a stark contrast to patients categorized under MetALD and MASLD who faced lower but still concerning risks.
The study, published in the esteemed journal Clinical Gastroenterology and Hepatology, revolved around a cohort consisting of diagnosed SLD patients juxtaposed against a healthy control group devoid of liver disease. Over a follow-up period of 4.5 years, 0.19% of participants were diagnosed with CRC. This was an alarming statistic that emphasizes the silent yet dangerous progression of the disease in this vulnerable patient population. The researchers asserted that disparities in CRC risk factors across SLD subgroups stem from their underlying pathophysiological mechanisms.
Alcohol, for instance, has been shown to contribute to colorectal carcinogenesis through various biochemical pathways. The development of toxic metabolites, along with resultant oxidative stress and subsequent DNA damage, serves to elevate the risk among heavy alcohol consumers and those with associated liver disease. Conjointly, MASLD, which is characterized by fatty liver associated with metabolic dysfunction, presents its unique challenges with increased inflammation and insulin resistance further augmenting the risk of CRC development.
In elucidating their study’s objectives, Dr. Kimura noted the importance of identifying high-risk patients belonging to the SLD demographic. He emphasized that by fostering awareness regarding their heightened risk for developing CRC, healthcare practitioners can promote routine screenings to facilitate early detection, which is pivotal for improving patient outcomes. Regular screening is not simply a recommendation; for this population, it becomes a necessity, as early diagnosis could drastically change the trajectory of colorectal cancer.
One possibly transformative outcome of this study is the potential for developing standardized screening protocols tailored specifically to the SLD subtypes, allowing healthcare systems to allocate resources effectively and intervene at an early stage. The implications of such an initiative extend beyond individual health outcomes, potentially alleviating the broader public health burden posed by colorectal cancer, which ranks among the leading causes of cancer-related morbidity and mortality.
CLR research illustrates that comprehensive screening and stratification strategies based on the newly recognized liver disease classifications could fundamentally reshape how clinicians approach disease management. The study authors advocate for a paradigm shift in how healthcare providers perceive the interconnections among alcohol consumption, metabolic dysfunction, and their collective impact on the risk for colorectal cancer. The emergence of tailored screening regimens could serve as a crucial public health measure to mitigate the late-stage presentations of cancers that are typically associated with poorer prognoses.
The revelations from this research are not only vital for clinical practice but also speak volumes about the escalating challenges posed by metabolic disorders and their comorbidities. For example, the study emphasizes the need for health education efforts targeting individuals with SLD, particularly as awareness surrounding the links between liver health and cancer risk is sorely lacking. This creates an opportunity for public health initiatives dedicated to ensuring that at-risk patients receive the knowledge and support necessary to take proactive measures regarding their health.
Furthermore, as researchers move forward, it is essential to monitor the long-term implications of these findings and the potential for integrating these insights into clinical guidelines for CRC screening. The collaboration between various institutions and the sharing of findings through reputable journals, such as Clinical Gastroenterology and Hepatology, indicates a commitment to advancing our understanding of complex disease relationships in the realm of liver health.
In conclusion, this landmark study by Dr. Kimura and colleagues not only unearths critical insights related to colorectal cancer and its ties to steatotic liver disease but also sets the stage for future research endeavors that could enhance cancer prevention and treatment strategies for affected populations. By emphasizing the interconnected aspects of liver disease and cancer risk, the study contributes to a broader understanding of chronic disease management and the necessity of proactive healthcare interventions.
Subject of Research: People
Article Title: Colorectal cancer incidence in steatotic liver disease (MASLD, MetALD, and ALD)
News Publication Date: 30-Jan-2025
Web References: Clinical Gastroenterology and Hepatology
References: DOI link
Image Credits: Dr. Takefumi Kimura from Shinshu University School of Medicine, Japan
Keywords: Colorectal cancer, steatotic liver disease, MASLD, metabolic dysfunction, ALD, MetALD, alcohol consumption, health outcomes, screening, public health.
Tags: alcohol-associated liver disease and healthcolorectal cancer and liver health connectioncolorectal cancer risk factorsepidemiological studies on liver diseasefatty liver disease and cancerliver disease and metabolic disordersmetabolic dysfunction-associated steatotic liver diseasenationwide study on colorectal cancernon-alcoholic fatty liver disease prevalencescreening for colorectal cancerSLD subtypes and cancer risktailored healthcare for liver disease patients