In the complex journey of cancer care, addressing the comprehensive needs of patients extends far beyond medical treatment alone. Recent research published in BMC Cancer shines a spotlight on the persistent and pervasive issue of unmet supportive care needs among cancer patients, a challenge that significantly affects patient well-being, treatment outcomes, and quality of life. This extensive study, conducted in Ethiopia, offers critical insights into the nature of these needs and the underlying factors influencing their prevalence, shedding light on crucial avenues for healthcare improvement and policy intervention.
Cancer care traditionally emphasizes diagnosis, treatment, and clinical management, but the multidimensional burdens patients endure are often underestimated. Unmet supportive care needs refer to the gaps in healthcare services and support systems that patients require but do not receive, encompassing physical, psychological, social, informational, and health system dimensions. Recognizing and quantifying these deficiencies is vital because they directly impact patient adherence to treatment, mental health status, and overall recovery trajectories.
The study adopted a rigorous cross-sectional design involving 260 cancer patients, reflecting a diverse representation across multiple cancer stages and demographic backgrounds. Employing a straightforward but effective random sampling methodology, the researchers meticulously collected data through validated instruments and ensured data integrity using advanced software tools such as EpiData and SPSS for thorough analysis. This methodological robustness strengthens the reliability of the findings and underscores the importance of data-driven decisions in oncology supportive care programming.
.adsslot_Pg1BfXQKhp{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_Pg1BfXQKhp{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_Pg1BfXQKhp{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
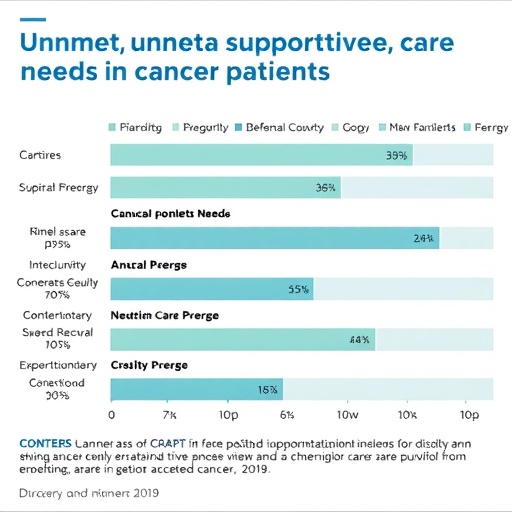
A striking finding from the research is the high prevalence of unmet supportive care needs, with nearly half of the respondents—45.9%—reporting at least one significant unmet need. This figure is both revealing and alarming, illustrating that existing healthcare structures are insufficient in meeting the holistic requirements of a substantial proportion of cancer patients. The pervasive nature of these unmet needs calls for urgent attention from healthcare providers, policymakers, and advocacy groups.
Among the spectrum of unmet needs identified, physical and health system needs emerged as the most prevalent. Physical needs encompass a range of symptoms and side effects related to cancer and its treatment, including pain, fatigue, and functional impairments, which often remain inadequately addressed. The prominence of health system needs points to systemic barriers such as accessibility, coordination of care, communication gaps, and resource limitations, which cumulatively hinder optimal patient support and satisfaction.
When diving deeper into the determinants of unmet supportive care needs, the analysis revealed that patient age, sex, educational attainment, and cancer stage at diagnosis are significant predictors. These factors illuminate the uneven distribution of support gaps and suggest targeted strategies to mitigate disparities. For instance, younger patients or those at advanced disease stages may require more intensive intervention efforts, while educational background could influence patients’ ability to seek help or navigate healthcare systems effectively.
The association between younger age and higher unmet needs might be interpreted through the lens of differing expectations and lifestyle impacts, as younger individuals often face unique challenges relating to employment, family roles, and psychosocial stressors. Gender differences in supportive care needs further complicate the landscape, possibly reflecting societal norms, communication patterns, and differential access to resources. Understanding these nuances is crucial for developing gender-sensitive and culturally appropriate care models.
Educational attainment serves as a proxy for health literacy and empowerment, influencing patients’ capacity to understand their illness, communicate effectively with providers, and advocate for necessary services. Lower educational levels may correlate with reduced awareness of available support options or hindered interactions with healthcare systems, exacerbating unmet needs. Therefore, patient education and navigation support should be integral components of care plans.
Cancer stage at diagnosis acts as an indicator of disease severity and complexity, with more advanced stages typically demanding comprehensive symptom management, palliative care, and psychosocial support. The study’s findings reinforce the necessity for stage-specific interventions, ensuring that patients at higher risk receive adequately tailored services that address their intensified needs.
This research is particularly critical in low-resource settings like Ethiopia, where healthcare infrastructure and supportive services face significant constraints. The insights gleaned demand not only clinical attention but also systemic reforms focusing on service delivery, workforce training, resource allocation, and policy frameworks that prioritize patient-centered care models. Addressing unmet supportive care needs is no longer a peripheral concern but a central pillar for improving cancer outcomes.
Moreover, the findings have broader implications for global oncology practice, highlighting universal challenges in supportive care delivery that transcend geographic and economic boundaries. They advocate for integrating comprehensive needs assessments into routine cancer care to identify gaps proactively and implement responsive interventions. Such integration requires multidisciplinary collaboration, technological innovation, and patient engagement strategies.
The study also exemplifies the role of rigorous quantitative research in unveiling complex healthcare issues. By employing logistic regression analyses, the researchers could isolate and quantify the impact of multiple variables simultaneously, providing a nuanced understanding of the interplay between demographic and clinical factors. This analytical approach strengthens the evidence base necessary for targeted program development.
Future directions prompted by this research include the development of culturally sensitive assessment tools, scalable supportive care interventions, and health policy reforms that embed supportive care as an essential component of cancer management. Education of healthcare providers about the importance of recognizing and responding to supportive care needs is equally vital to translating research into practice.
Technological advancements such as telemedicine, digital health platforms, and mobile health applications can also be leveraged to bridge the gaps in supportive care, especially in underserved areas. Innovative solutions might enhance communication, follow-up, and resource accessibility, thereby reducing unmet needs efficiently and cost-effectively.
In conclusion, the research underscores a pressing, yet often overlooked, facet of cancer care—the unmet supportive care needs that compromise patient well-being and treatment efficacy. By illuminating the scope and determinants of these needs among Ethiopian cancer patients, the study paves the way for informed interventions and policy measures aimed at optimizing supportive care delivery. The ultimate goal is to transform cancer care into a truly holistic endeavor that empowers patients, supports recovery, and enhances quality of life across all stages of the disease.
Subject of Research: Unmet supportive care needs and associated factors among cancer patients
Article Title: Unmet supportive care need and associated factors among cancer patients
Article References:
Mehari, W.D., Sun, Y., Lei, Y. et al. Unmet supportive care need and associated factors among cancer patients.
BMC Cancer 25, 1260 (2025). https://doi.org/10.1186/s12885-025-14607-w
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14607-w
Tags: cancer patient well-beingcancer treatment outcomes and quality of lifecomprehensive cancer careEthiopian cancer care researchhealth system challenges in cancer carehealthcare improvement and policy intervention in cancermultidimensional burdens of cancerpatient adherence to cancer treatmentpsychological needs in cancer treatmentsocial support for cancer patientssupportive care gaps in healthcareunmet supportive care needs in cancer patients