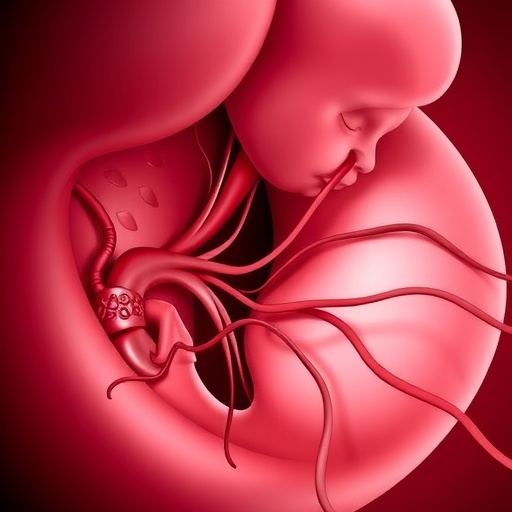
In the intricate dance of pregnancy, one of the most alarming yet often underrecognized complications is fetomaternal hemorrhage (FMH), a condition in which fetal blood cells cross into the maternal circulation. This phenomenon, when clinically significant, poses grave risks to the newborn, challenging obstetricians and neonatologists alike. A groundbreaking review published in the Journal of Perinatology sheds light on the complex pathogenesis, diagnostic challenges, and management strategies of FMH, highlighting why early recognition is vital in saving newborn lives and reducing morbidity.
Fetomaternal hemorrhage occurs when fetal blood escapes through the placental barrier and enters the mother’s bloodstream, occurring in varying degrees throughout pregnancy. While minor occurrences can be clinically silent and often go unnoticed, large volume FMH close to childbirth can trigger acute fetal distress. In these critical moments, the infant may suffer from profound hypovolemia, shock, and life-threatening metabolic imbalances, which can escalate to encephalopathy if not promptly identified and managed.
Clinicians have long grappled with the elusive nature of FMH, compounded by its diverse presentations. Acute FMH typically manifests in the peripartum period when placental integrity is compromised, possibly due to trauma, invasive procedures, or placental abruption. The rapid loss of fetal blood volume in these cases precipitates hypoxic injury, demanding immediate intervention. Conversely, chronic FMH, characterized by a slow and sustained leakage of fetal erythrocytes, unfolds insidiously, often detected only after signs of fetal anemia or heart failure emerge.
The pathophysiology of FMH is multifaceted, involving the disruption of the placental barrier’s delicate architecture. Normally, fetal and maternal blood remain separated by trophoblastic layers and vascular endothelium. However, mechanical injury, inflammatory processes, or abnormalities in placental vasculature can breach this barrier. Once fetal cells infiltrate the maternal circulation, they can be rapidly cleared, but extensive hemorrhage overwhelms maternal compensatory mechanisms and precipitates fetal compromise.
Diagnosing FMH before delivery remains a daunting clinical challenge. Traditional laboratory tests, such as the Kleihauer-Betke test, detect fetal erythrocytes in maternal blood by exploiting differences in hemoglobin composition. Although widely used, this test suffers from interobserver variability and limited sensitivity, often underestimating fetal blood volume loss. Innovations in flow cytometry and molecular diagnostics have improved precision but are not yet universally accessible, underscoring a significant gap in FMH detection.
From a clinical perspective, the consequences of unrecognized or untreated FMH are dire. Acutely affected neonates may face hypovolemic shock requiring aggressive volume resuscitation and blood transfusions immediately after birth. Metabolic acidosis, a marker of oxygen deprivation, can lead to multi-organ dysfunction or permanent neurologic damage. In contrast, chronic FMH prompts a different clinical picture, where the fetus adapts by ramping up erythropoiesis, resulting in compensatory hepatomegaly and heart failure, culminating in hydrops fetalis if untreated.
Management protocols for FMH are continually evolving, directed by advances in prenatal imaging and fetal medicine. Doppler ultrasonography has emerged as a non-invasive beacon, detecting elevated peak systolic velocities in the middle cerebral artery – a proxy for fetal anemia. This technique enables early intervention, such as intrauterine transfusions, potentially averting severe anemia or hydrops. However, these interventions require meticulous timing and specialized expertise, highlighting the necessity for multidisciplinary prenatal care teams.
Despite these strides, substantial knowledge gaps persist. There remains no consensus on screening measures for asymptomatic patients, nor on the threshold of fetal blood loss that mandates intervention. Furthermore, the long-term neurodevelopmental outcomes of infants who survive significant FMH are not fully elucidated, calling for rigorous longitudinal studies to inform counseling and therapeutic strategies.
The review also underscores the maternal implications of FMH, which include sensitization to fetal antigens and the risk of alloimmunization complicating future pregnancies. This adds a layer of complexity in managing at-risk mothers, advocating for tailored monitoring and prophylactic measures. Advanced immunologic assays may soon refine maternal risk stratification, but their integration into clinical practice awaits validation.
Innovation in FMH research continues with promising molecular biomarkers on the horizon. These biomarkers aim to detect subtle placental leaks and fetal distress before clinical symptoms manifest. Coupled with artificial intelligence algorithms analyzing ultrasonographic data, these technologies promise a paradigm shift from reactive to predictive management of FMH, ultimately transforming neonatal outcomes.
Beyond diagnostics and treatment, public health efforts must emphasize awareness and education regarding FMH. Given its potential for sudden catastrophic events during labor or delivery, frontline healthcare workers require training to recognize early signs and implement emergency protocols swiftly. Collaborative efforts between obstetricians, neonatologists, hematologists, and laboratory scientists are essential for advancing care.
In summation, clinically significant fetomaternal hemorrhage represents a perilous interplay between mother and fetus that, if undetected, can result in devastating neonatal consequences. This comprehensive review offers a timely synthesis of current understanding, highlighting the urgent need for improved diagnostic tools, standardized management guidelines, and robust research to bridge existing knowledge gaps. As the field accelerates towards precision medicine, practitioners are hopeful that these advances will herald a new era in safeguarding newborns from the silent threat of FMH.
Subject of Research: Fetomaternal hemorrhage – pathogenesis, diagnosis, clinical management, and outcomes
Article Title: Fetomaternal hemorrhage: pathogenesis, diagnosis, and clinical management
Article References: Sankaran, D., Giusto, E., Lim, M.J. et al. Fetomaternal hemorrhage: pathogenesis, diagnosis, and clinical management. J Perinatol (2026). https://doi.org/10.1038/s41372-025-02548-y
Image Credits: AI Generated
DOI: 05 January 2026
Keywords: fetomaternal hemorrhage, fetal anemia, neonatal hypovolemia, placental pathology, perinatal diagnostics, intrauterine transfusion, neonatal outcomes, obstetric emergencies
Tags: acute fetal distress during labordiagnosis of fetomaternal hemorrhageearly recognition of FMHfetal blood circulation complicationsfetomaternal hemorrhage causeshypovolemia and shock in neonatesinterventions for fetomaternal hemorrhagemanagement strategies for FMHmaternal-fetal medicine challengesperipartum complications in pregnancyplacental barrier integrity issuesrisks of FMH in newborns