Credit: Karen Moxon/UC Davis
Engineers at the University of California, Davis, will lead a consortium of universities, biomedical startups and nonprofit organizations to develop interventions for spinal cord injuries that can be applied within days of injury to improve long-term outcomes.
Karen Moxon, professor of biomedical engineering at UC Davis, will lead the five-year, $36 million contract as part of the Defense Advanced Research Project Agency, or DARPA, Bridging the Gap Plus Program. A primary goal is to develop technologies to stabilize a patient’s hemodynamic response, which includes blood flow and blood pressure, within days of injury.
Because large swings in blood pressure are common following spinal cord injuries, stabilizing hemodynamics within days of injury will improve functional recovery. The team will take advantage of stabilized hemodynamics to optimize delivery of neural stem cells using personalized 3D printed scaffolds within two weeks of injury to regenerate lost connections within the injured spinal cord.
“Spinal cord injury is a complex condition that causes partial or complete loss of function below the location of injury,” Moxon said. “We will develop systems for real-time biomarker monitoring and intervention to stabilize and rebuild neural communications pathways between the brain and spinal cord. As a result of our efforts, clinicians will be able to collect previously unavailable diagnostic information for automated or clinician-directed interventions. Our goal is to translate these technologies to humans within the five-year award period.”
The international team includes 12 institutions: UC Davis, UC San Diego, UC San Francisco, the University of British Columbia, the University of Calgary and the École Polytechnique Fédérale de Lausanne (EPFL, Switzerland); biotech startups Pathonix Innovation Inc. of Vancouver, GTX Medical (Lausanne, Switzerland), and Teliatry (Richardson, Texas); nonprofit institutions the Wyss Center for Bio and Neuroengineering (Geneva, Switzerland) and Battelle Memorial Institute (Columbus, Ohio); and a regulatory consultant firm, NetValue BioConsulting Inc., Toronto.
Moxon and her team at UC Davis — including Zhaodan Kong, associate professor in the Department of Mechanical and Aerospace Engineering, and Professor Kiarash Shahlaie and Assistant Professor Julius Ebinu, neurosurgeons in the UC Davis School of Medicine — will take the lead on assessing the impact of these interventions on the brain to maximize the restoration of both motor and sensory functions. This part of the project will be conducted at the California National Primate Research Center.
“We are extremely pleased that the California National Primate Research Center will host the nonhuman primate research arm of this extraordinary effort to restore function following spinal cord injury,” said center director John Morrison, professor of neurology at UC Davis.
Part of the effort will also aim to improve functional recovery, using neural stem cell and bioengineering scaffold technology developed by professors Mark Tuszynski, Paul Lu, Ephron Rosenzweig and Jacob Koffler, all faculty in the Department of Neurosciences at UCSD. Their stem cell and scaffold technology will be combined with neural electrical stimulation technology (“neuromodulation”) developed by Gregoire Courtine at EPFL. The team hopes to successfully combine this cell and engineering technology to promote nerve regeneration that bridges the injury site.
Advancing key technologies
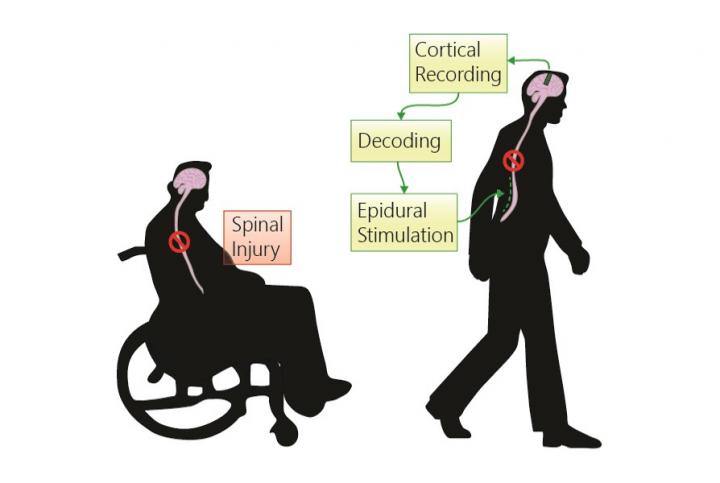
Moxon’s lab at UC Davis, in collaboration with a team at the Wyss Center for Bio and Neuroengineering led by Tracy Laabs, will develop cortical stimulation protocols to enhance sensory feedback to the brain and aid in motor control. The team will take advantage of Wyss’s ABILITY system that wirelessly records signals from individual neurons in the brain and will further develop it to include closed-loop cortical stimulation, which employs a sensor to record signals, for improved motor function.
The multi-institution team will focus on advancing three main technologies:
- A near-infrared spectroscopy sensor, developed by University of British Columbia spine surgeon Brian Kwon, co-principal investigator, and commercialized by Pathonix Innovations Inc., to assess blood oxygenation and blood flow at the site of spinal injury
- A fully implantable mean arterial pressure sensor that will be developed by a team of scientists including Aaron Phillips at the University of Calgary, Dane Grasse at Teliatry and Andrew Schimmoeller at Battelle
- A system to stimulate the spinal cord and regulate blood pressure developed by Courtine and his team at EPFL, which is being commercialized by GTX Medical.
Together, these technologies will integrate into a system-of-systems that monitors the information from sensors and stimulators to allow clinicians to monitor patients’ progress. At the same time, the team will be able to identify the optimal time to transplant the neural stem cells and 3D scaffold in this critical time period after injury.
“It is exciting to lead this talented team of international scientists and to be in a position to effect real change for people who sustain a spinal cord injury,” Moxon said. “It’s this type of team science between academia and industry that makes clinical breakthroughs possible in short time periods.”
###
Development of the proposal for the award was facilitated by the UC Davis Office of Research’s Interdisciplinary Research Support team and Gabriela Lee, project manager. This project is part of a larger effort at UC Davis led by Moxon, Professor Sanjay Joshi in the Department of Mechanical and Aerospace Engineering, and Professor Carolynn Patten in the School of Medicine and College of Biological Sciences to develop a neuroengineering program that aims to restore, augment and extend human capacity to benefit society.
Media Contact
Andy Fell
[email protected]
Original Source
https:/




