An institutional effort to reduce the amount of opioids prescribed following lumbar surgery
Credit: © 2018 American Association of Neurological Surgeons.
CHARLOTTESVILLE, VA (FEBRUARY 5, 2019). As we all know, opioid addiction in the US has reached epidemic proportions. In 2017 alone, opioids were involved in the overdose deaths of 47,600 people. Many victims of opioid abuse began their journey with physician-prescribed medications that initially were provided for the management of acute or chronic pain. Often the source of this pain is damage to the lumbar spine or a temporary side effect of lumbar spine surgery.
Physicians and medical institutions are actively seeking solutions to lower the risks of opiate addiction. One focus is reducing the amounts of opioids that are initially prescribed for patients in acute pain. Excess opioid medication has the potential to lead to addiction in patients or misuse by family members or others with access to leftover opioid pills.
At Hospital for Special Surgery (HSS) in New York City (ranked Number 1 in orthopedics 2018-19 by U.S. News & World Report), a task force developed a 1-hour educational program on opiate use and misuse, the role of the orthopedic prescriber, multimodal analgesia, and state laws regarding opioid prescription. All opioid prescribers at the institution were mandated to attend the program in person or via an online presentation. A committee composed of spine surgeons, pain management physicians, anesthesiologists, and nurse managers established guidelines for prescribing opioids following spine surgery. These qualitative guidelines, based on individual patients’ consumption of opioids while in the hospital, were disseminated throughout the hospital early in 2017.
In the article “An institutional intervention to modify opioid prescribing practices after lumbar spine surgery,” published today in the Journal of Neurosurgery: Spine, Francis Lovecchio, MD, and colleagues address the question of whether this intervention–mandatory provider education together with prescription guidelines–could change prescriber behavior, resulting in a lower amount of opioids prescribed at hospital discharge after lumbar surgery.
Lovecchio and colleagues compared opioid prescription data in the electronic medical records of 1177 patients treated by lumbar surgery before the intervention (March 1-November 1, 2016) with similar data in the electronic medical records of 1302 patients treated after the intervention (February 1-October 1, 2017). Because a variety of opioid medications with different strengths had been prescribed, the researchers converted the amount of opioid per prescription into an oral morphine equivalent (OME) to make comparisons possible.
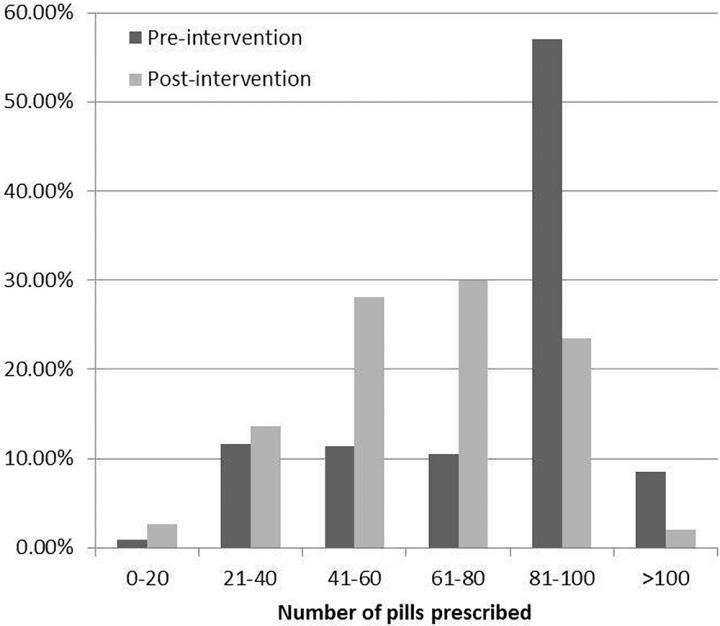
The researchers found a statistically significant reduction in both the mean amount of opioid (629 ± 294 OME pre-intervention vs. 490 ± 245 OME post-intervention, p
The researchers estimate that in the 8 months following dissemination of the guidelines, “the change in prescribing practices may have saved the dispensing of over 26,000 narcotic pills.”
Lovecchio and colleagues show how the intervention at HSS changed prescriber behavior, resulting in a lower amount of prescribed opioids. They suggest that future studies should be undertaken to focus on how these changes in prescriber behavior may affect patient outcomes.
When asked about the importance of the study, Dr. Lovecchio said, “While we have been able to show that qualitative prescribing guidelines work to change prescriber behavior, the most practical solution to overprescribing is to define the ‘minimum necessary quantity’ of opioid to prescribe for the average patient after a given spine procedure. This will prove challenging, as postoperative opioid consumption likely depends on a complex interplay of biological, psychosocial, and surgery-related factors, and patient expectations. Our group and many others are working toward this end, and I look forward to finding solutions.”
###
Lovecchio F, Stepan JG, Premkumar A, Steinhause ME, Sava M, Derman P, Kim HJ, Albert T: An institutional intervention to modify opioid prescribing practices after lumbar surgery. J Neurosurg Spine, published ahead of print February 5, 2019. DOI: 10.3171/2018.8.SPINE18386.
Disclosure: Dr. Albert has been a consultant for NuVasive, Facet Link, Zimmer Biomet, and DePuy Synthes; receives royalties from JP Medical Publishers, Saunders/Mosby-Elsevier, Zimmer Biomet, DePuy Synthes, and Thieme; has served on the Medical Advisory Board for Gentis and United Health Care; has ownership in United Health Care; has direct stock ownership in Gentis, Vital 5, Bonovo Orthopedics Inc., Biomerix, InVivo Therapeutics, Spinicity, Crosstrees Medical, Paradigm Spine LLC, Invuity, ASIP, PMIG, and Pioneer; is an employee of Weill Cornell Medical College; has received support from PCORI, NIH, and ISSG for non-study-related clinical or research effort; and is the president of the Scoliosis Research Society and the past president of the Cervical Spine Research Society.
Drs. Lovecchio, Stepan, Premkumar, Steinhaus, Kim, and Albert and Ms. Sava are affiliated with the Hospital for Special Surgery, New York, NY; Dr. Derman is affiliated with Midwest Orthopaedics at Rush, Chicago, IL.
For additional information, contact: Ms. Jo Ann M. Eliason, Communications Manager, JNS Publishing Group, One Morton Drive, Suite 200, Charlottesville, VA 22903; Email [email protected]; Phone 434-982-1209.
The Journal of Neurosurgery: Spine is a monthly peer-reviewed journal focused on neurosurgical approaches to treatment of diseases and disorders of the spine. It contains a variety of articles, including descriptions of preclinical and clinical research as well as case reports and technical notes. The Journal of Neurosurgery: Spine is one of four monthly journals published by the JNS Publishing Group, the scholarly journal division of the American Association of Neurological Surgeons. Other peer-reviewed journals published by the JNS Publishing Group each month include the Journal of Neurosurgery, Neurosurgical Focus, and the Journal of Neurosurgery: Pediatrics. All four journals can be accessed at http://www.
Founded in 1931 as the Harvey Cushing Society, the American Association of Neurological Surgeons (AANS) is a scientific and educational association with more than 10,000 members worldwide. The AANS is dedicated to advancing the specialty of neurological surgery in order to provide the highest quality of neurosurgical care to the public. All active members of the AANS are certified by the American Board of Neurological Surgery, the Royal College of Physicians and Surgeons (Neurosurgery) of Canada or the Mexican Council of Neurological Surgery, AC. Neurological surgery is the medical specialty concerned with the prevention, diagnosis, treatment and rehabilitation of disorders that affect the entire nervous system including the brain, spinal column, spinal cord, and peripheral nerves. For more information, visit http://www.
Media Contact
Jo Ann M. Eliason
[email protected]
434-982-1209
Related Journal Article
http://dx.




