In the realm of hematological malignancies, diffuse large B-cell lymphoma (DLBCL) represents a formidable challenge due to its heterogeneous nature and variable clinical outcomes. Recent insights from a pivotal study by Zhang et al. have shed light on the critical role of the TP53 gene mutation, unveiling its significant association with poor prognostic outcomes in affected patients. This research highlights the necessity for further exploration into genetic markers that can enhance understanding and treatment modalities for DLBCL.
The TP53 gene is often referred to as the “guardian of the genome,” serving a vital role in regulating cell division and maintaining genomic stability. When mutations occur within this gene, the consequences can be dire. The research conducted by Zhang and colleagues underscores the need for a closer examination of TP53 mutations within DLBCL cohorts. Their findings potentially herald a new era in tailoring therapy based on genomic alterations, thus paving the way for personalized medicine in oncology.
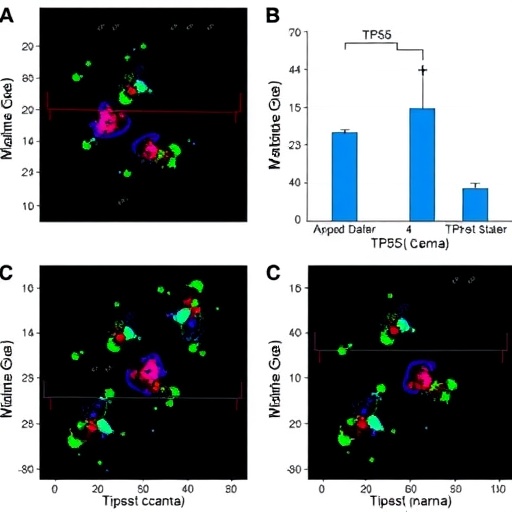
The study, carried out at a single center, meticulously analyzed a cohort of DLBCL patients, identifying the prevalence and impact of TP53 mutations on treatment outcomes. This rigorous investigation involved a comprehensive review of clinical, pathological, and genetic data. The results of this study boldly assert that the presence of TP53 mutations significantly correlates with adverse survival outcomes. This relationship accentuates the urgency for clinicians to consider genetic profiling as part of the standard diagnostic work-up for DLBCL.
Moreover, understanding the implications of TP53 mutations could reshape therapeutic strategies. It has been established that DLBCL is treatable, yet prognosis remains stubbornly variable. The findings from Zhang et al. suggest that patients with TP53 mutations may require more aggressive treatment protocols and closer monitoring due to their higher propensity for relapse and poorer overall survival rates. This revelation could lead to a paradigm shift in how healthcare professionals approach DLBCL therapy.
Importantly, the implications of TP53 mutations extend beyond mere prognostication. They could serve as actionable targets for innovative therapeutic interventions. The burgeoning field of precision medicine has made it increasingly apparent that tailored approaches based on an individual’s genetic makeup can yield more effective outcomes. By stratifying patients based on TP53 mutation status, clinicians could implement targeted therapies that specifically address the underlying genetic aberrations.
In addition to therapeutic implications, the study has considerable ramifications for patient counseling and shared decision-making in DLBCL management. Knowledge of a patient’s TP53 status could empower individuals to make informed choices regarding their treatment plans. Discussions around the potential need for escalated treatment regimens, clinical trial opportunities, and supportive care measures are paramount as clinicians navigate the complex landscape of DLBCL care.
Furthermore, the broader implications of these findings reach into the domains of research and clinical trials. As awareness grows regarding the significance of TP53 mutations, researchers may seek to incorporate this data into future clinical trials, ultimately refining eligibility criteria and treatment regimens. The alignment of molecular characteristics with therapeutic ethics warrants a deeper investigation within the scientific community, as the quest for more effective strategies to combat DLBCL gains momentum.
As we delve deeper into the complexities of cancer genomics, the work of Zhang et al. serves as a testament to the importance of integrative approaches in cancer research. Their study not only emphasizes the role of TP53 as a crucial biomarker but also highlights the intricate interplay between genetics and clinical outcomes. The medical community is urged to embrace such developments, as they represent a leap toward harnessing the full potential of personalized oncology.
Ultimately, the journey sparked by this research is far from over. Ongoing studies must explore the mechanistic pathways through which TP53 mutations exert their influence on DLBCL biology. In parallel, collaborations among multidisciplinary teams can foster innovative approaches to treatment, incorporating insights from genomics into clinical practice. The commitment to unraveling the complexities of DLBCL will be instrumental in bringing forth hope for patients facing this challenging diagnosis.
As this research echoes throughout the medical community, it urges all stakeholders to remain vigilant. The potential to alter the trajectory of treatment for DLBCL patients lies within our grasp. With each study, we inch closer to the goal of a future where genomics not only informs diagnosis but also revolutionizes treatment paradigms, improving outcomes for countless individuals navigating the turbulent waters of lymphoma.
In conclusion, the study by Zhang et al. serves as a clarion call for the integration of genetic testing into routine practice for DLBCL. The TP53 mutation emerges as a powerful prognostic indicator, casting a wide net of implications for patient care and research. As we embark on this journey, the hope is that with continued exploration and collaboration, we will unveil new strategies that empower patients and transform the landscape of lymphoma management for the better.
Subject of Research: TP53 mutation in diffuse large B-cell lymphoma
Article Title: TP53 mutation predict poor prognosis in diffuse large B-cell lymphoma: a single-center study.
Article References:
Zhang, H., Zhang, X., Wang, J. et al. TP53 mutation predict poor prognosis in diffuse large B-cell lymphoma: a single-center study. Ann Hematol 105, 66 (2026). https://doi.org/10.1007/s00277-026-06821-8
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00277-026-06821-8
Keywords: TP53 mutation, diffuse large B-cell lymphoma, prognosis, genetics, personalized medicine.
Tags: cancer treatment modalities advancementcell division regulation in lymphomasclinical outcomes of DLBCLdiffuse large B-cell lymphoma prognosisDLBCL patient cohort studygenetic markers in DLBCLgenomic alterations in cancergenomic stability in cancerhematological malignancies researchpersonalized medicine in oncologyTP53 gene mutationsTP53 mutations impact on treatment