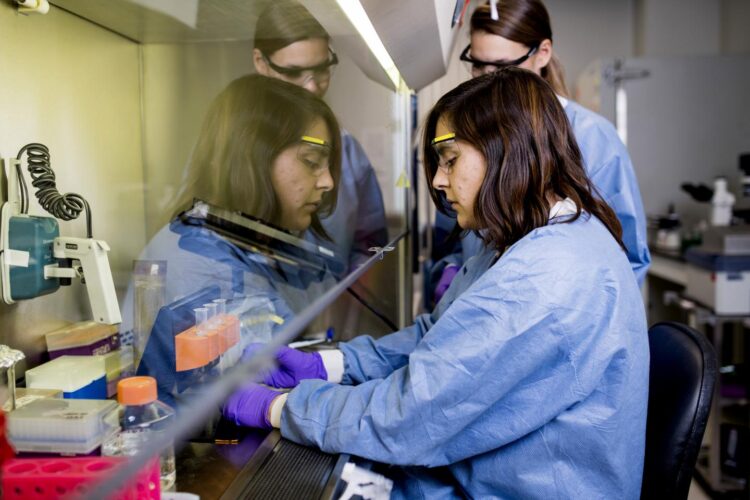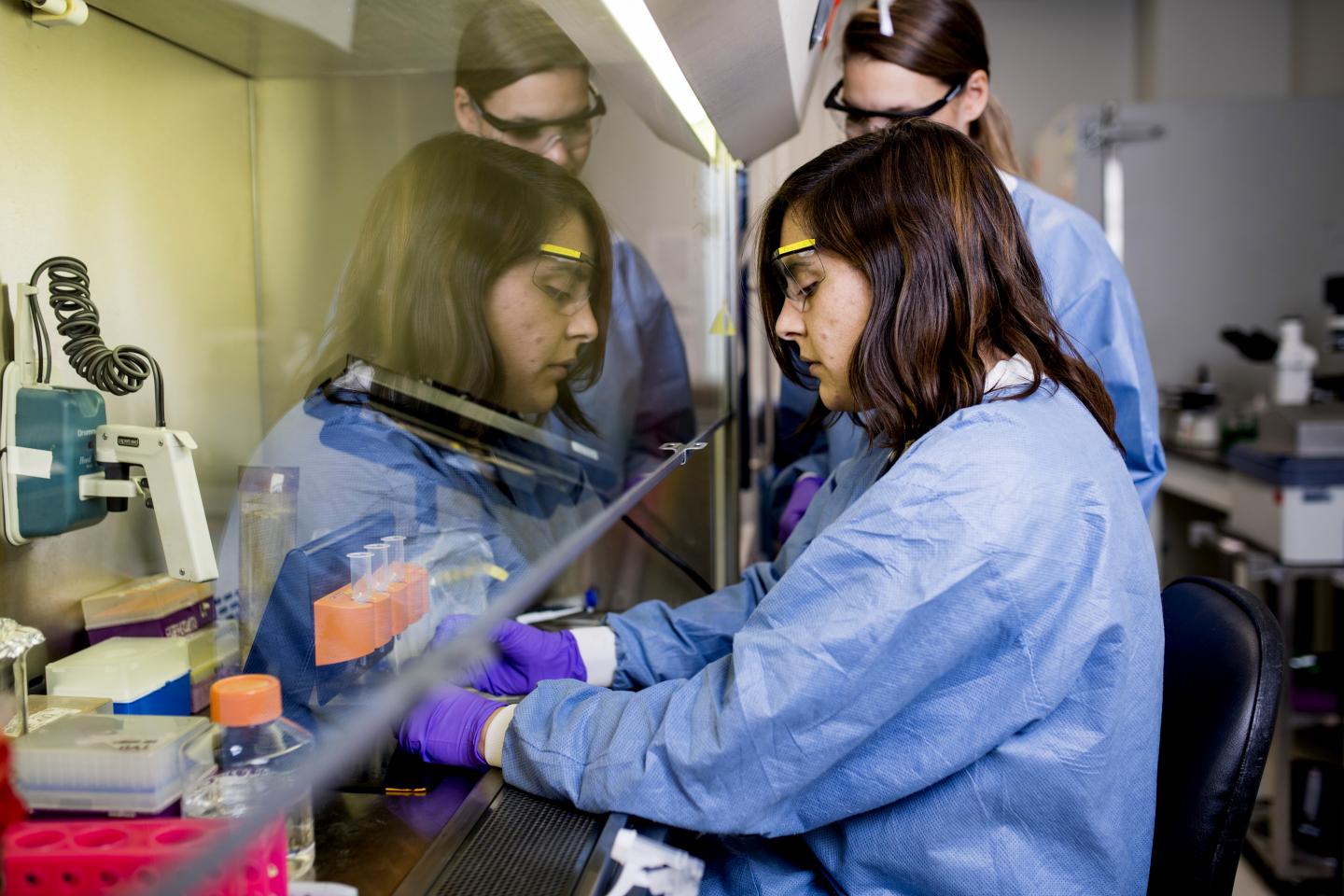
Credit: Matthew Modoono/Forsyth Institute
In diseases characterized by bone loss -such as periodontitis, rheumatoid arthritis, and osteoporosis- there is a lot that scientists still don’t understand. What is the role of the immune response in the process? What happens to the regulatory mechanisms that protect bone?
In a paper published recently in Scientific Reports, researchers from the Forsyth Institute and the Universidad de Chile describe a mechanism that unlocks a piece of the puzzle. Looking at periodontal disease in a mouse model, scientists found that a specific type of T cell, known as regulatory T cells, start behaving in unexpected ways. These cells lose their ability to regulate bone loss and instead begin promoting inflammation.
“That is important because, in many therapies analyzed in in-vivo models, researchers usually check if the number of regulatory T cells has increased. But they should check if these cells are indeed functioning,” says Dr. Carla Alvarez, a postdoctoral researcher at Forsyth and lead author of the paper.
Regulatory T cells control the body’s immune response. In periodontal disease, bone loss occurs because the body’s immune system responds disproportionately to the microbial threat, causing inflammation and destroying healthy tissue. Normally, regulatory T cells help suppress that destruction, but they appear to lose their suppressive abilities during periodontal disease.
In scientific terms, this process is analyzed in the field of osteoimmunology, which explores the complex interactions between the immune system and bone metabolism.
“This is an interesting mechanism highlighting how the bone loss is taking place in periodontal disease,” says Dr. Alpdogan Kantarci, Senior Member of Staff at Forsyth and co-author of the paper together with Dr. Rolando Vernal, Professor from the School of Dentistry at Universidad de Chile.
In the case of periodontal disease, a potential therapy targeting regulatory T cells could restore the T cells’ normal functioning, not just increase their numbers.
“Unfortunately, this is not a linear process–that’s the complicated part,” Kantarci says.
Periodontal disease is initiated by microbes in the mouth, making it all the more complex.
“The relationship between immune response and bone is not so straightforward,” says Alvarez. “There are multiple components. You have to imagine a complex network of signaling and cells that participate.”
This cellular and microbial complexity is what makes the disease so difficult to study in humans. However, examining this mechanism in humans is the next step of the research, Alvarez says. The research team is planning a collaborative study to look at healthy and diseased patients, intending to observe similar mechanisms to what was seen in the animal model.
###
Media Contact
Alexandra Nicodemo
[email protected]
Original Source
https:/