NIH study shows specific set of immune cells can harm and also help brain after injury
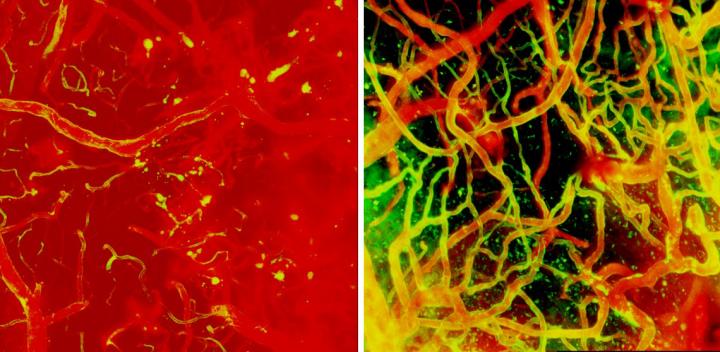
Credit: Image credit: McGavern Lab/NINDS.
Researchers from the National Institutes of Health have discovered Jekyll and Hyde immune cells in the brain that ultimately help with brain repair but early after injury can lead to fatal swelling, suggesting that timing may be critical when administering treatment. These dual-purpose cells, which are called myelomonocytic cells and which are carried to the brain by the blood, are just one type of brain immune cell that NIH researchers tracked, watching in real-time as the brain repaired itself after injury. The study, published in Nature Neuroscience, was supported by the National Institute of Neurological Disorders and Stroke (NINDS) Intramural Research Program at NIH.
“Fixing the brain after injury is a highly orchestrated, coordinated process, and giving a treatment at the wrong time could end up doing more harm than good,” said Dorian McGavern, Ph.D., NINDS scientist and senior author of the study.
Cerebrovascular injury, or damage to brain blood vessels, can occur following several conditions including traumatic brain injury or stroke. Dr. McGavern, along with Larry Latour, M.D., NINDS scientist, and their colleagues, observed that a subset of stroke patients developed bleeding and swelling in the brain after surgical removal of the blood vessel clot responsible for the stroke. The swelling, also known as edema, results in poor outcomes and can even be fatal as brain structures become compressed and further damaged.
To understand how vessel injury can lead to swelling and to identify potential treatment strategies, Dr. McGavern and his team developed an animal model of cerebrovascular injury and used state-of-the-art microscopic imaging to watch how the brain responded to the damage in real-time.
Immediately after injury, brain immune cells known as microglia quickly mobilize to stop blood vessels from leaking. These “first responders” of the immune system extend out and wrap their arms around broken blood vessels. Dr. McGavern’s group discovered that removing microglia causes irreparable bleeding and damage in the brain.
A few hours later, the damaged brain is invaded by circulating peripheral monocytes and neutrophils (or, myelomonocytic cells). As myelomonocytic cells move from the blood into the brain, they each open a small hole in the vasculature, causing a mist of fluid to enter the brain. When thousands of these cells rush into the brain simultaneously, a lot of fluid comes in all at once and results in swelling.
“The myelomonocytic cells at this stage of repair mean well, and do want to help, but they enter the brain with too much enthusiasm. This can lead to devastating tissue damage and swelling, especially if it occurs around the brain stem, which controls vital functions such as breathing,” said Dr. McGavern.
After this initial surge, the monocytic subset of immune cells enter the brain at a slower, less damaging rate and get to work repairing the vessels. Monocytes work together with repair-associated microglia to rebuild the damaged vascular network, which is reconnected within 10 days of injury. The monocytes are required for this important repair process.
In the next set of experiments, Dr. McGavern and his colleagues tried to reduce secondary swelling and tissue damage by using a combination of therapeutic antibodies that stop myelomonocytic cells from entering the brain. The antibodies blocked two different adhesion molecules that myelomonocytic cells use to attach to inflamed blood vessels. These were effective at reducing brain swelling and improving outcomes when administered within six hours of injury.
Interestingly, the therapeutic antibodies did not work if given after six hours or if they were given for too long. In fact, treating mice over a series of days with these antibodies inhibited the proper repair of damaged blood vessels, leading to neuronal death and brain scarring.
“Timing is of the essence when trying to prevent fatal edema. You want to prevent the acute brain swelling and damage, but you do not want to block the monocytes from their beneficial repair work,” said Dr. McGavern.
Plans are currently underway for clinical trials to see if administering treatments at specific timepoints will reduce edema and brain damage in a subset of stroke patients. Future research studies will examine additional aspects of the cerebrovascular repair process, with the hope of identifying other therapeutic interventions to promote reparative immune functions.
###
This study was supported by the NINDS Intramural Research Program.
Reference:
Mastorakos P. et al. Temporally Distinct Myeloid Cell Reponses Mediate Damage and Repair After Cerebrovascular Injury. Nature Neuroscience. January 18 2021.
For more information, please visit:
ninds.nih.gov
https:/
The NINDS is the nation’s leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.
About the National Institutes of Health (NIH): NIH, the nation’s medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit http://www.
Media Contact
Barbara McMakin
[email protected]




