New data on telemedicine use by adults over 50 show change since previous poll in 2019, including reduced worries about privacy and virtual interaction

Credit: University of Michigan
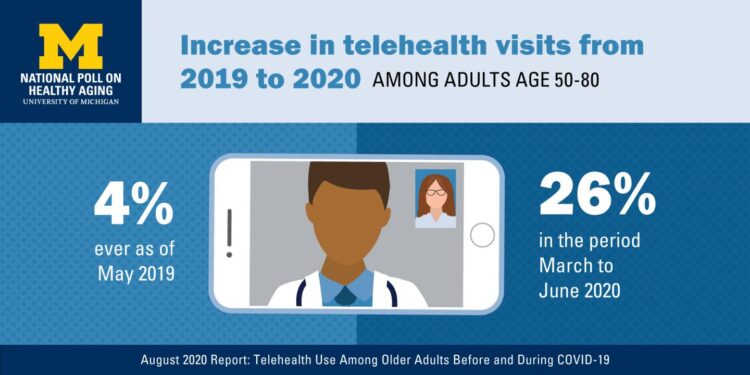
One in four older Americans had a virtual medical visit in the first three months of the COVID-19 pandemic, most of them by video, a new telehealth poll finds. That’s much higher than the 4% of people over 50 who said they had ever had a virtual visit with a doctor in a similar poll taken in 2019.
Comfort levels with telehealth, also called telemedicine, have also increased. Back in 2019, most older adults expressed at least one serious concern about trying a telehealth visit. But by mid-2020, the percentage with such concerns had eased, especially among those who had experienced a virtual visit between March and June of this year.
Yet not all older adults see virtual care as an adequate substitute for in-person care, even in a pandemic, the National Poll on Healthy Aging findings show.
And 17% of people over 50 still say they have never used any sort of video conferencing tool for any reason, including medical care. While that’s 11 percentage points lower than in the 2019 poll, that lack of experience or access could be a barrier to receiving care without having to leave home as the pandemic continues to surge in dozens of states.
Both the 2019 and 2020 polls were done for the University of Michigan’s Institute for Healthcare Policy and Innovation with support from AARP and Michigan Medicine, U-M’s academic medical center. Both involved a national sample of more than 2,000 adults aged 50 to 80.
“These findings have implications for the health providers who have ramped up telehealth offerings rapidly, and for the insurance companies and government agencies that have quickly changed their policies to cover virtual visits,” says Laurie Buis, Ph.D., M.S.I., a health information technology researcher at U-M who helped design the poll and interpret its results. “Tracking change over time could inform future efforts, and highlights the need for much more research on concerns, barriers and optimal use of telehealth by older adults.”
“This has been an extraordinary time for the telemedicine movement, and these poll results show just how powerful this ‘trial by fire’ has been,” says Jeff Kullgren, M.D., M.P.H., M.S., associate director of the poll, health care researcher and a primary care provider who uses telehealth with his patients at the VA Ann Arbor Healthcare System. “But our data also highlight areas of continued concern for patients that need to be addressed.”
COVID-19 impacts
The poll finds that 30% older adults had ever participated in a telehealth visit by June 2020, perhaps reflecting changes in insurance coverage that began to take effect before the pandemic. But the figure for March through June suggests that much of the movement to telehealth visits resulted from states mandating reductions in elective and non-emergency health care during the first months of the pandemic, as part of “stay home” public health requirements aimed at reducing the spread of the virus.
Nearly half of those who had had a telehealth visit said that they had had an in-person visit canceled or rescheduled by their health care provider between March and June, and 30% said that a virtual visit was the only option when they called to schedule an appointment.
Awareness about the special risks of COVID-19 among older adults may have also played a role, as 45% of respondents said the pandemic made them more interested in telehealth. The percentage was higher among those who had had a telehealth visit in the past. But only 15% of the poll respondents who had a telehealth visit said that fear of the virus led them to request a telehealth visit, whether for a new concern or in place of a previously scheduled visit.
Among those who had telehealth visit this past spring, 91% said it was easy to connect with their doctor. One-third had their visits via a video connection from their phone, and another third carried out the video visit on a tablet or computer. In addition, 36% had an audio-only visit by phone, which the 2019 poll did not ask about.
Year-over-year change
The new poll asked older adults many of the same questions as the poll conducted in 2019. This allows for comparisons between the two years, such as the percentage who said:
- They feel very or somewhat comfortable with video conferencing technologies: 64%, up from 53% in 2019
- At least one of their health providers offer telehealth visits: 62%, up from 14%
* They are interested in using telehealth to connect with a provider they had seen before: 72%, up from 58% - They are interested in using telehealth for a one-time follow-up appointment after a procedure or operation: 63%, up from 55%
- They have concerns about privacy during a telehealth visit: 24%, down from 49%
- They are concerned they would have difficulty seeing or hearing the provider during a video visit: 25%, down from 39%
But there was almost no change in the percentage who said they would feel comfortable seeing a provider for the first time via a virtual visit (about one in three would), and the percentage who felt that the quality of care in a telehealth visit was not as good (about two-thirds).
Moving forward
Physician groups, insurers, professional societies and organizations including AARP are monitoring the situation with telehealth, and in some cases advocating for the temporary changes in Medicare and Medicaid payment policy, and other relevant regulations, to become permanent.
In June, AARP Research released a report about older adults’ awareness of and attitudes toward telehealth. AARP has also published resources to help older adults and their caregivers use telehealth services.
“It’s clear from this study and AARP’s research that older adults are increasingly comfortable with telehealth and are willing to use technology to interact with their health providers,” says Alison Bryant, Ph.D., senior vice president of research for AARP, says. “As the coronavirus pandemic continues, telehealth has been a useful tool for older adults to access health care from the safety of their own homes, but we must be mindful that not everyone can access these services.”
Meanwhile, Buis is leading a new COVID-19-related telehealth research interest group as part of a broader IHPI initiative to evaluate the impacts and appropriate use of telehealth as well as barriers. Buis is an assistant professor in the U-M Department of Family Medicine, which has pivoted to virtual care for many primary care appointments along with the rest of Michigan Medicine.
The National Poll on Healthy Aging results are based on responses from a nationally representative sample of 2,074 adults aged 50 to 80 who answered a wide range of questions online. Questions were written, and data interpreted and compiled, by the IHPI team. Laptops and Internet access were provided to poll respondents who did not already have them.
###
A full report of the findings and methodology is available at http://www.
Media Contact
Kara Gavin
[email protected]