In a groundbreaking advance emerging from the Virginia Commonwealth University (VCU) Massey Comprehensive Cancer Center, researchers have uncovered a pivotal molecular mechanism that drives the debilitating and common side effect of chemotherapy-induced peripheral neuropathy (CIPN). Published in the prestigious journal Brain, Behavior and Immunity, this new study reveals how the tumor-promoting gene Astrocyte Elevated Gene-1 (AEG-1) acts not just in cancer progression but also as a master regulator of inflammation processes leading to CIPN. This discovery paves the way for novel, targeted therapies that could dramatically improve quality of life for millions of cancer patients suffering from the painful neurological complications of chemotherapy.
Chemotherapy-induced peripheral neuropathy remains a persistent clinical challenge, affecting an estimated 30% of cancer patients undergoing treatment with platinum-based agents and taxanes – two commonly used chemotherapy drug classes. Characterized by tingling, numbness, and debilitating pain in the extremities, CIPN results from nerve damage caused by systemic inflammation triggered during chemotherapy. Current clinical management strategies are woefully insufficient, lacking any FDA-approved medications specifically designed to prevent or treat CIPN. Often, oncologists are forced to reduce chemotherapy dosage or cease regimen altogether to spare patients from unbearable pain, leading to suboptimal cancer control.
Central to the new findings is AEG-1, a gene historically recognized for its oncogenic role in tumorigenesis and cancer progression. This gene orchestrates inflammatory signaling pathways and tumor growth, making it a key player in cancer biology. While AEG-1’s involvement in fatty liver disease and hepatic cancers has been extensively studied over the past two decades, its direct impact on chemotherapy-induced neuroinflammation and peripheral neuropathy had remained unexplored until now. The research team hypothesized that AEG-1 expressed in immune cells, specifically myeloid-lineage cells, could mediate the inflammatory cascade underlying CIPN.
.adsslot_LcwaTZKFiz{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_LcwaTZKFiz{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_LcwaTZKFiz{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
By leveraging sophisticated preclinical models, the scientists selectively deleted AEG-1 in myeloid cells and observed a striking inhibition of chemotherapy-induced neuroinflammation. This genetic manipulation effectively prevented the development of the neuropathic symptoms associated with CIPN. The findings suggest that AEG-1’s activity in this subset of immune cells is not merely correlative but causal in the onset of chemotherapy-associated nerve damage. These preclinical results open a promising therapeutic window to target AEG-1 for CIPN prevention without compromising cancer treatment efficacy.
The study’s lead authors emphasize the critical unmet medical need their research addresses. Dr. M. Imad Damaj, a professor of pharmacology and toxicology at the VCU School of Medicine, explained that no current pharmaceutical agent accurately targets CIPN mechanisms linked to inflammation. He envisions that inhibiting AEG-1 activity can form the basis of a revolutionary class of therapeutics offering an alternative to opioids, which remain the current mainstay of CIPN pain relief despite their addictive potential and limited long-term efficacy.
Nervous system damage in CIPN involves complex crosstalk between peripheral nerves and the immune system, leading to persistent neuroinflammation. Chemotherapy agents such as taxanes and platinum compounds induce cytokine release and activation of inflammatory myeloid cells that exacerbate nerve injury. The discovery of AEG-1’s regulatory role within these immune populations provides a molecular target to quell this damaging inflammatory milieu. By silencing AEG-1 specifically in myeloid cells, the study demonstrated reduced inflammatory signaling and preservation of nerve function in treated animals.
Associate director for research training and education at Massey, Dr. Devanand Sarkar, also a professor of cellular, molecular, and genetic medicine, highlighted that targeting AEG-1 capitalizes on decades of knowledge regarding its role in inflammation-driven tumor progression. Beyond CIPN, blocking AEG-1 could present a dual-action strategy to not only mitigate chemotherapy neurotoxicity but also inhibit tumor growth, offering a holistic approach to cancer therapy. The implications for survivorship and enhanced quality of life in cancer patients could be revolutionary.
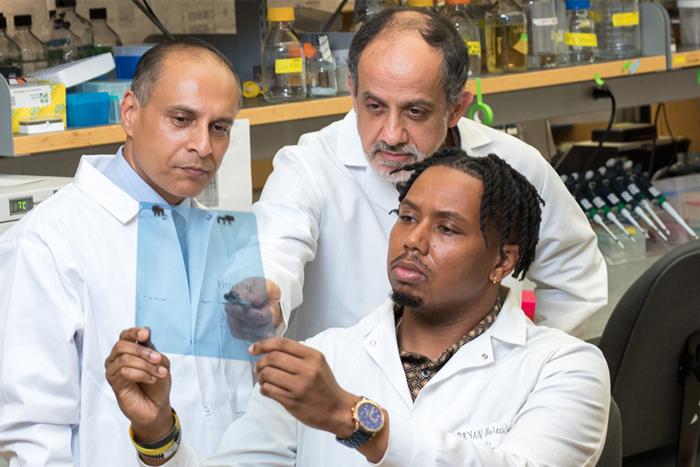
Co-author Bryan McKiver, Ph.D., now a postdoctoral associate at Yale University, underscored the translational potential of these findings. The next logical step involves developing pharmacological inhibitors of AEG-1 that can be tested in clinical trials to assess their efficacy in preventing CIPN in humans. Moreover, future investigations will seek to answer whether AEG-1-targeted therapies can reverse established neuropathy, a complex clinical problem still lacking effective solutions.
The research team included other experts across multiple institutions, integrating expertise from cancer biology, pharmacology, and immunology. Collaborators from VCU’s School of Medicine and the University of Iowa supported this multidisciplinary effort, highlighting the importance of immune cell regulation not only in cancer treatment side effects but also in broader contexts of tumor immunity and inflammation. This networked approach exemplifies modern biomedical innovation.
Chemotherapy-induced peripheral neuropathy represents a critical barrier to effective cancer treatment, often impairing patients’ functionality and long-term well-being. Additionally, CIPN-related dose reductions and discontinuations compromise therapeutic outcomes, contributing to poor cancer prognoses. By unveiling a novel molecular driver of CIPN, the study advances our understanding of chemotherapy side effects at the intersection of oncology and immunology and identifies actionable targets for intervention.
In conclusion, the identification of AEG-1 as a key mediator of neuroinflammation in myeloid cells sets the stage for transformative clinical strategies in managing CIPN. As the global cancer burden continues to rise, therapies that both enhance treatment tolerability and maintain oncologic efficacy are paramount. The VCU Massey research team’s work offers a beacon of hope for the development of safer, targeted treatments that could alleviate neuropathic suffering and optimize cancer care, marking a promising horizon for patients and clinicians alike.
Subject of Research: Animals
Article Title: Astrocyte elevated gene-1 (AEG-1) in myeloid cells is a key driver for the development of chemotherapy-induced peripheral neuropathy
News Publication Date: 22-Mar-2025
Web References:
https://www.sciencedirect.com/science/article/pii/S0889159125001059?via%3Dihub
DOI link: http://dx.doi.org/10.1016/j.bbi.2025.03.020
Image Credits: VCU Massey Comprehensive Cancer Center
Keywords: Neuropathic pain, Chemotherapy, Cancer medication
Tags: AEG-1 gene in cancerchemotherapy side effects managementchemotherapy-induced peripheral neuropathyFDA-approved medications for CIPNimproving quality of life for cancer patientsinflammation regulation in CIPNneurological complications of chemotherapynovel treatments for cancer painplatinum-based chemotherapy agentstargeted therapies for nerve paintaxanes and nerve damageVCU Massey Comprehensive Cancer Center research