In search of better cancer treatments, researchers at Washington University School of Medicine in St. Louis have designed synthetic molecules that combine the advantages of two experimental RNA therapies.
RNA is closely related to DNA and plays an important role in how genes are turned on and off in the body. Both siRNAs and microRNAs are snippets of RNA known to modulate a gene’s signal or shut it down entirely. Separately, siRNA and microRNA treatment strategies are in early clinical trials against cancer, but few groups have attempted to marry the two.
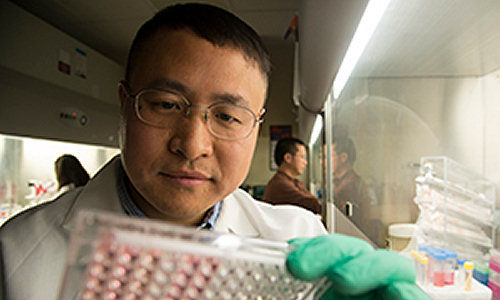
“These are preliminary findings, but we have shown that the concept is worth pursuing,” said Xiaowei Wang, PhD, assistant professor of radiation oncology at the School of Medicine and a research member of the Siteman Cancer Center. “We are trying to merge two largely separate fields of RNA research and harness the advantages of both.”
The study appears in the December issue of the journal RNA.
“We designed an artificial RNA that is a combination of siRNA and microRNA,” Wang said. “Working with cancer cells in the laboratory, we showed that our artificial RNA combines the functions of the two separate molecules, simultaneously inhibiting both cell migration and proliferation.”
For therapeutic purposes, “small interfering” RNAs, or siRNAs, are designed and assembled in a lab and can be made to shut down – or interfere with – a single specific gene that drives cancer.
The siRNA molecules work extremely well at silencing a gene target because the siRNA sequence is made to perfectly complement the target sequence, thereby silencing a gene’s expression. Though siRNAs are great at turning off the gene target, they also have potentially dangerous side effects: siRNAs inadvertently can shut down other genes that need to be expressed to carry out tasks that keep the body healthy.
According to Wang and his colleagues, siRNAs interfere with off-target genes that closely complement their “seed region,” a short but important section of the siRNA sequence that governs binding to a gene target.
“We can never predict all of the toxic side effects that we might see with a particular siRNA,” said Wang. “In the past, we tried to block the seed region in an attempt to reduce the side effects. Until now, we never tried to replace the seed region completely.”
Wang and his colleagues asked whether they could replace the siRNA’s seed region with the seed region from microRNA. Unlike siRNA, microRNA is a natural part of the body’s gene expression. And it can also shut down genes. As such, the microRNA seed region (with its natural targets) might reduce the toxic side effects caused by the artificial siRNA seed region. Plus, the microRNA seed region would add a new tool to shut down other genes that also may be driving cancer.
Wang’s group started with a bioinformatics approach, using a computer algorithm to design siRNA sequences against a common driver of cancer, a gene called AKT1 that encourages uncontrolled cell division. They used the program to select siRNAs against AKT1 that also had a seed region highly similar to the seed region of a microRNA known to inhibit a cell’s ability to move, thus potentially reducing the cancer’s ability to spread. In theory, replacing the siRNA seed region with the microRNA seed region also would combine their functions – reducing cell division and movement with a single RNA molecule.
Of more than 1,000 siRNAs that can target AKT1, they found only three that each had a seed region remarkably similar to the seed region of the microRNA that reduces cell movement.
They then took the microRNA seed region and used it to replace the seed region in the three siRNAs that target AKT1. The close similarity between the two seed regions is required because changing the original siRNA sequence too much would make it less effective at shutting down AKT1.
They dubbed the resulting combination RNA molecule “artificial interfering” RNA, or aiRNA. Once they arrived at these three sequences using computer models, they actually assembled the aiRNAs and tested them in cancer cells.
One of the three artificial RNAs that they built in the lab combined the advantages of the original siRNA and the microRNA seed region that was transplanted into it. This aiRNA greatly reduced both cell division (like the siRNA) and movement (like the microRNA). And to further show proof-of-concept, they also did the reverse, designing an aiRNA that both resists chemotherapy and promotes movement of the cancer cells.
“Obviously, we would not increase cell survival and movement for cancer therapy, but we wanted to show how flexible this technology can be, potentially expanding it to treat diseases other than cancer,” Wang said.
Story Source:
The above story is based on materials provided by Washington University School of Medicine.