In a groundbreaking development for the treatment and evaluation of multiple myeloma (MM), a novel patient-centered endpoint called symptomatic progression-free survival (SPFS) has emerged, promising a more comprehensive understanding of the patient experience beyond traditional clinical measures. This innovative approach integrates disease progression with patient-reported outcomes (PROs), providing a nuanced, holistic metric that better reflects how patients live with and respond to the disease.
Multiple myeloma, a complex hematological malignancy characterized by the uncontrolled proliferation of plasma cells, has traditionally been monitored using progression-free survival (PFS) as a primary endpoint. While PFS effectively measures the interval during which the disease does not worsen, it does not capture the quality of life or symptom burden experienced by patients. Recognizing this critical gap, researchers turned their attention to creating a composite endpoint that merges clinical data with symptomatic insights, aiming to address the patient perspective head-on.
Central to the development of this endpoint was a comprehensive systematic literature review (SLR), which synthesized symptom data across 34 publications to identify those most relevant to MM patients. The exhaustive review extracted 16 distinct symptoms associated with disease progression and patient well-being. These symptoms were then meticulously evaluated by a Delphi panel of experts, a method that harnesses collective intelligence to reach consensus, ultimately narrowing down the most clinically impactful patient experiences.
.adsslot_XhLJBIwAV9{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_XhLJBIwAV9{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_XhLJBIwAV9{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
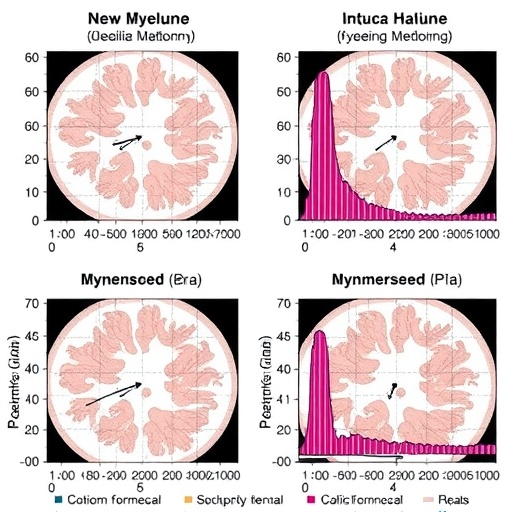
The Delphi panel identified four key symptoms — drowsiness, fatigue, pain, and poor mobility — that are intimately linked to disease progression and represent significant detriments to patient quality of life. Among these, three symptoms demonstrated a statistically significant correlation with progression-free survival outcomes: pain, fatigue, and poor mobility. Each of these was measured on a 100-point scale, where a 10-point worsening corresponded with a substantive increase in risk of disease progression — 22% for pain, 20% for fatigue, and 31% for poor mobility.
Using these insights, the research team conducted a sophisticated post-hoc analysis of data from the MagnetisMM-3 trial, which investigated elranatamab, an innovative therapy for MM. This analysis underscored the value of incorporating patient-reported symptom worsening within a 28-day window as a component of the SPFS composite endpoint, thus linking subjective symptomatic changes directly with objective disease progression or death events.
The use of SPFS as a clinical endpoint represents a paradigm shift in oncological research, particularly for MM. By embedding patient-reported outcomes alongside traditional measures, SPFS provides a richer and more precise framework for evaluating therapeutic efficacy. This integration allows clinicians to capture subtle but meaningful declines in patient function and well-being that may precede or coincide with measurable disease progression.
Such a patient-centered approach not only enhances the accuracy of clinical trials but also paves the way for more tailored treatment strategies. Patients experiencing worsening symptoms on the SPFS scale may be identified earlier for intervention, potentially enhancing quality of life and overall treatment responsiveness. This shifts clinical decision-making to a more proactive and individualized model, where patient voice and data converge.
Moreover, SPFS could serve as a valuable endpoint in future drug development, regulatory approvals, and real-world clinical practice. Its dual focus on survival and symptomatology aligns well with the increasing emphasis on value-based care and personalized medicine, where outcomes meaningful to patients are prioritized alongside traditional metrics.
The findings from the MagnetisMM-3 trial secondary analysis also contribute to a growing recognition that clinical progression alone does not encapsulate the entirety of the MM patient journey. Symptoms such as fatigue and mobility challenges can profoundly affect everyday life, underscoring the need for tools that integrate these experiences into endpoints that drive research and treatment.
Notably, median SPFS was not reached at the time of analysis, with a 95% confidence interval spanning from 12.2 months to not reached, suggesting promising durability of symptom stability or disease control under elranatamab therapy. This further emphasizes the potential utility of SPFS in capturing long-term patient outcomes.
As MM therapies evolve rapidly with the introduction of novel agents and immunotherapies, endpoints like SPFS that encompass patient-reported outcomes become increasingly crucial for distinguishing treatment benefit. They provide a richer narrative that goes beyond tumor markers or imaging, placing patient experience at the forefront of clinical assessment.
The research advocates for broader adoption of SPFS in clinical trials and encourages its consideration as a standard measure in MM management protocols. Incorporating this composite endpoint into future studies could standardize how patient-reported symptoms influence clinical evaluation and regulatory pathways.
Ultimately, the advent of SPFS symbolizes a transformative acknowledgment that measuring survival without considering symptomatic experience offers an incomplete picture of patient health. It reflects a movement toward truly patient-centric oncology, where scientific rigor and empathetic care coexist and advance together.
This comprehensive integration of symptomatic dynamics into progression metrics promises to reshape MM research, fostering innovations not only in drug efficacy evaluations but also in enhancing patient quality of life worldwide. With SPFS, the field steps closer to treatments that are measured not just by longevity but by lived experience.
Symptomatic progression-free survival represents a critical evolution in cancer research methodology, highlighting the indispensable role of patient-reported outcomes in crafting meaningful, actionable healthcare insights. It sets a precedent, inviting similar approaches across other malignancies where symptom burden intricately weaves with disease progression.
As the field looks ahead, continued refinement of SPFS and validation across diverse patient populations will be essential. Embracing such patient-centered endpoints will deepen our understanding of cancer’s impact, guiding the next generation of therapies and care standards.
Subject of Research: Patient-centered clinical endpoints in multiple myeloma integrating patient-reported symptoms with progression-free survival.
Article Title: Symptomatic progression-free survival as an emerging patient-centered endpoint in multiple myeloma: a secondary analysis of MagnetsiMM-3 trial data
Article References:
Kortüm, M., Theurich, S., Farrell, J. et al. Symptomatic progression-free survival as an emerging patient-centered endpoint in multiple myeloma: a secondary analysis of MagnetsiMM-3 trial data. BMC Cancer 25, 1288 (2025). https://doi.org/10.1186/s12885-025-14724-6
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14724-6
Tags: clinical measures vs patient experiencecomposite endpoints in cancer researchexpert consensus in symptom evaluationhematological malignancies evaluationintegration of patient-reported outcomesmultiple myeloma treatment advancementspatient-centered healthcare metricsprogression-free survival limitationsquality of life in multiple myelomasymptomatic progression-free survivalsystematic literature review in oncologyunderstanding patient symptom burden