In recent years, neonatal encephalopathy resulting from suspected hypoxic–ischaemic encephalopathy (HIE) has emerged as a critical subject of investigation in perinatal medicine. This condition, marked by brain dysfunction due to oxygen deprivation and impaired blood flow around the time of birth, remains a leading cause of neonatal morbidity and mortality worldwide. Insights from a groundbreaking new study published in World Journal of Pediatrics — authored by Horn, Pillay, Velaphi, and colleagues — are poised to deepen scientific understanding and reshape therapeutic approaches toward this devastating neurological disorder.
Neonatal encephalopathy is characterized by a broad spectrum of neurobehavioral abnormalities, ranging from altered consciousness and impaired respiration to seizures and motor deficits. The pathophysiology of hypoxic–ischaemic events lies at the intersection of complex metabolic, cellular, and inflammatory cascades triggered by oxygen and blood flow deprivation. These insults result in neuronal necrosis and apoptosis, reactive gliosis, excitotoxicity, and oxidative stress, revealing a multifactorial process that challenges clinicians and researchers alike.
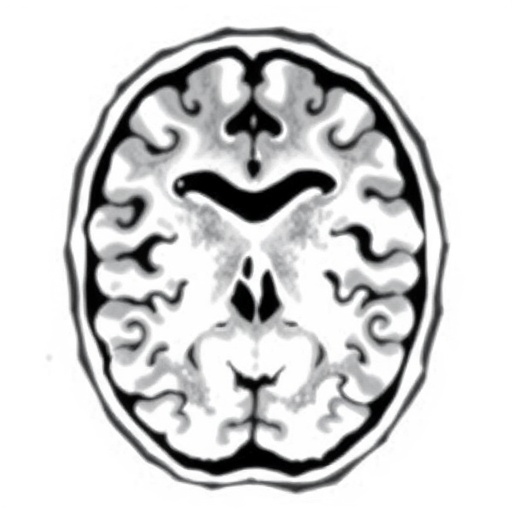
The study harnesses innovative diagnostic techniques to refine the identification of infants most at risk. Traditional clinical assessments and biochemical markers have faced limitations due to their subjective nature and delayed release patterns. However, the utilization of novel neuroimaging modalities, particularly diffusion-weighted magnetic resonance imaging (DW-MRI) combined with advanced spectroscopy methods, affords a more precise localization and visualization of injury patterns. This technological evolution in neurodiagnostics holds promise for earlier, targeted interventions, potentially mitigating long-term impacts.
.adsslot_9QZsuCIO4K{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_9QZsuCIO4K{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_9QZsuCIO4K{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Moreover, functional assessments of cerebral autoregulation and oxygen cerebral extraction, measured through non-invasive cerebral oximetry, are leveraged to detect critical fluctuations in cerebral hemodynamics during the perinatal period. This approach offers a real-time window into the evolving brain injury landscape, enabling clinicians to tailor therapeutic hypothermia and adjunct neuroprotective treatments dynamically.
Neuroinflammation occupies a central role in the progression from initial injury to sustained neuronal damage in hypoxic–ischaemic encephalopathy. The authors stress that activation of microglia and astrocytes, coupled with infiltration of peripheral immune cells, orchestrate a detrimental inflammatory milieu. Inflammatory cytokines such as interleukin-1β, tumor necrosis factor-α, and interleukin-6 exacerbate excitotoxic conditions and blood-brain barrier disruption. Understanding these immune pathways illuminates novel targets for pharmacological modulation in the clinical setting.
In parallel, the study highlights the importance of mitochondrial dysfunction as a key driver of energy failure within affected neurons. Oxygen deprivation impairs oxidative phosphorylation, leading to the accumulation of reactive oxygen species and consequent mitochondrial permeability transition pore opening. This cascade culminates in cytochrome c release and caspase activation, precipitating programmed cell death. Targeting mitochondrial resilience emerges as a promising therapeutic frontier in HIE management.
Therapeutic hypothermia, currently the gold standard for treating moderate to severe hypoxic–ischaemic encephalopathy, mitigates metabolic rate and inflammatory responses, evidently improving neurodevelopmental outcomes. However, the study emphasizes existing gaps in efficacious treatment for mild HIE cases and the potential scope to enhance hypothermia protocols by integrating adjuvant agents. Pharmacotherapies aimed at blocking excitotoxic pathways and modulating neuroinflammation are undergoing rigorous evaluation.
A particularly intriguing development reported involves stem cell therapy, which holds transformative potential for repairing damaged neural tissue. Multipotent mesenchymal stem cells demonstrated immunomodulatory and regenerative capacities in preclinical studies, fostering neurovascular remodeling and attenuating apoptosis. Clinical trials are increasingly incorporating these strategies, yet ethical considerations and long-term safety profiles remain under scrutiny.
The socioeconomic impact of HIE cannot be understated, as affected infants often require prolonged hospitalizations, intensive care, and rehabilitative services, placing a substantial burden on healthcare systems worldwide. The research underscores the pressing need for prenatal risk stratification and timely intrapartum monitoring to prevent hypoxic episodes, thereby reducing disease incidence and improving resource allocation.
The integration of artificial intelligence and machine learning algorithms in diagnostic imaging and predictive modeling is another cutting-edge element discussed. By harnessing vast datasets, these technologies enable pattern recognition beyond human capability, allowing for individualized risk assessment and personalized medicine approaches. Such innovations promise to revolutionize neonatal care pathways in the near future.
Furthermore, the study delves into epigenetic modifications induced by hypoxic stress, shedding light on gene expression changes that influence neural plasticity and susceptibility to injury. Methylation patterns and microRNA profiles emerge as molecular signatures potentially serving as biomarkers for prognosis and therapeutic response monitoring. This genomic perspective enriches the multidimensional understanding of HIE pathogenesis.
The global disparities in perinatal outcomes related to hypoxic–ischaemic encephalopathy are apparent, with resource-limited settings disproportionately affected. The authors advocate for scalable and cost-effective screening tools, alongside international collaborations, to bridge these gaps. Capacity-building in neonatal care units and education of healthcare providers are emphasized as critical steps toward reducing neonatal encephalopathy burden.
Importantly, long-term follow-up studies detailed in this research underscore the challenges in predicting neurodevelopmental trajectories. Cognitive impairments, motor disabilities, epilepsy, and behavioral disorders can manifest years after the initial insult. Early intervention programs combining physical therapy, cognitive rehabilitation, and family support systems play vital roles in optimizing quality of life for survivors.
Subject of Research: Neonatal encephalopathy caused by suspected hypoxic–ischaemic encephalopathy
Article Title: Neonatal encephalopathy due to suspected hypoxic–ischaemic encephalopathy
Article References:
Horn, A.R., Pillay, S., Velaphi, S. et al. Neonatal encephalopathy due to suspected hypoxic–ischaemic encephalopathy.
World J Pediatr (2025). https://doi.org/10.1007/s12519-025-00952-0
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s12519-025-00952-0
Tags: brain dysfunction in newbornshypoxic-ischaemic encephalopathy researchinnovative diagnostic techniques in neonatologymetabolic and inflammatory cascadesneonatal encephalopathyneonatal morbidity and mortalityneurobehavioral abnormalities in infantsneuroimaging in neonatal careneuronal necrosis and apoptosis in infantspathophysiology of hypoxic-ischaemiaperinatal medicine advancementstherapeutic approaches for HIE