Physician education, monitoring, and incentives lead to a shift from longer-term to shorter-term prescriptions for surgical patients, according to new Journal of the American College of Surgeons study
Credit: American College of Surgeons
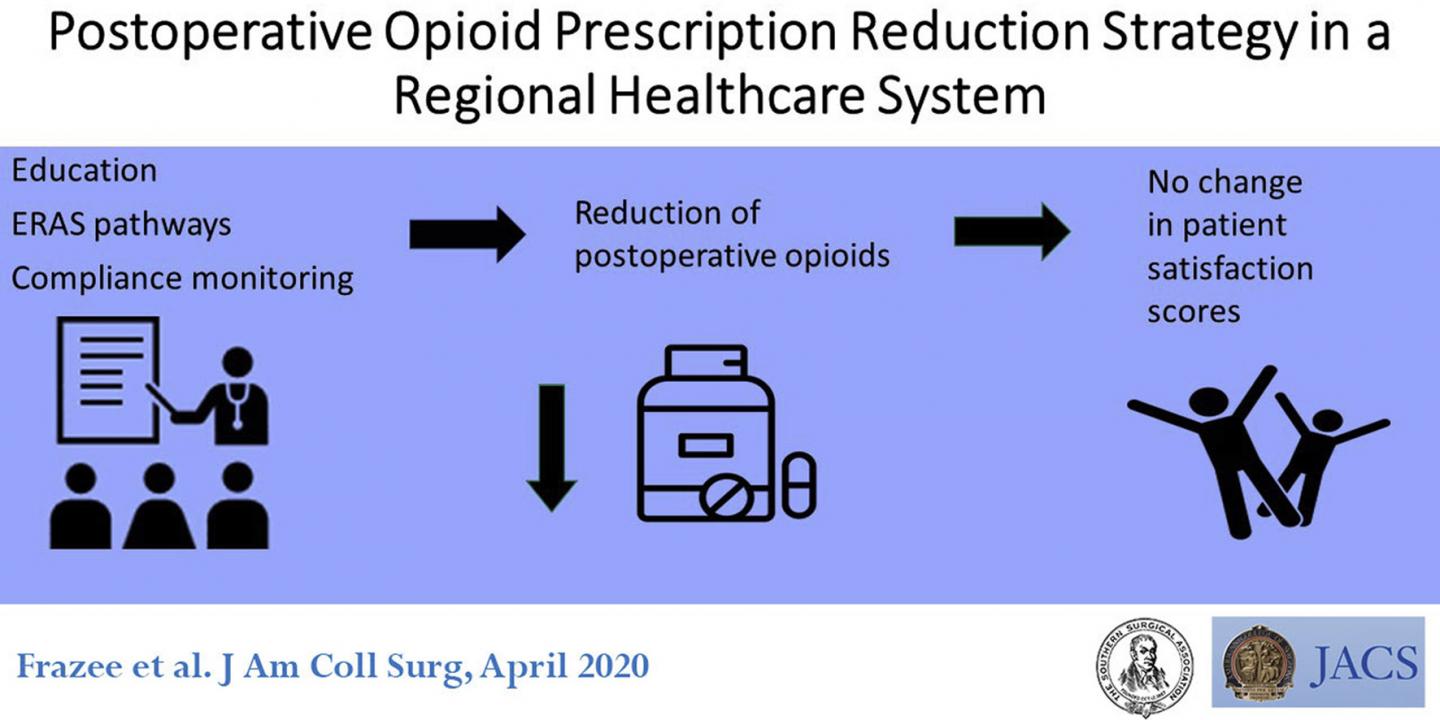
CHICAGO (March 2, 2020): Opioid prescriptions have been a known driver of the opioid epidemic, and it’s now known that opioid prescriptions that last longer than five days are a risk factor for longer-term opioid use.1 As some surgeons’ prescribing patterns have been found to be part of the problem, the surgical community is now working hard to address it. A recent solution has been enacted by a large health-care system in central Texas, where surgeons implemented a pain management program that reduced longer-term prescriptions by two-thirds, according to a study published as an “article in press” on the Journal of the American College of Surgeons website ahead of print.
The program reduced postsurgery opioid prescriptions at Baylor Scott &White (BSW) hospitals of more than five days by 64 percent, from 1,228 in the three months before the program started to 432 in the first three months of 2019. Prescriptions of less than five days duration increased 15 percent, from 5,133 to 5,923. Baylor Scott & White in central Texas consists of 15 hospitals, 104 clinics, and 1,543 physicians. Overall, BSW encompasses 50 hospitals, more than 7,800 physicians, and 5,100 patient beds.
“Opioid prescriptions of over five days have been shown to dramatically increase addiction to opioids,” said lead study author Richard Frazee, MD, FACS, a general surgeon at Baylor Scott & White Healthcare in Temple, Texas. “We established a standard of opioid prescriptions of five days or less after elective surgery.”
The program consisted of using the monthly surgical grand rounds–a conference of a hospital’s physicians, residents and medical students–to educate surgeons and anesthesiologists about the opioid epidemic and how postsurgery opioid prescriptions contributed to it. At these meetings, the rationale for limiting opioid prescriptions to five days or less was introduced. The program also used the electronic health record (EHR) to monitor each physician’s opioid prescribing practices and, after six months, tied this measure to the quality component of their compensation.
Overall, the study included 31,814 patients who had elective surgery at the hospitals from January 2018, when the program began, through March 2019. Over the five quarters the study observed, a greater proportion of opioid prescriptions shifted from more than five days to fewer than five days.
Changing the way surgeons prescribe pain medication after surgery was not easy, Dr. Frazee acknowledged. The researchers noted that surgeons’ prescribing patterns have been slow to respond nationally to the opioid crisis, citing a Kaiser Health News-Johns Hopkins analysis2 that found that surgeons frequently wrote prescriptions of 100 pills or more from 2011 to 2016. “As always, to change surgeons’ behavior you have to convince them that it is a benefit to their patients,” he said. “We had to overcome many years of misinformation on the ‘safety’ of liberal use of opioids after surgery.”
The program is one that can easily be used in other hospitals and health systems, Dr. Frazee said. “This is an issue that health-care providers and the public are increasingly aware of,” he said. “The Baylor Scott & White Healthcare System has adopted and emphasized a culture of safety. This program offers a model for other health-care systems and individual surgeons to adopt in the care of their patients.”
But tackling opioid addiction requires a multipronged approach. “The opioid crisis is ongoing; this study is one step in the process to addressing it,” Dr. Frazee said. “A continued multipronged approach is needed that incorporates education, pharmaceutical reform, rehabilitation programs, and easy disposal of unneeded prescriptions.”
###
Study coauthors are Emily Garmon, MD, of the department of anesthesia; Erin Bird, MD, MBA, of the department of urology; and Claire Isabel, MD, FACS, and Harry Papaconstantinou, MD, FACS, of the department of surgery at Baylor Scott & White Healthcare in Temple, Texas.
“FACS” designates that a surgeon is a Fellow of the American College of Surgeons.
The authors have no relevant financial disclosures.
The study was originally presented at the Southern Surgical Association 131st annual meeting, Hot Springs, Virginia, December 2019.
Citation: Postoperative Opioid Prescription Reduction Strategy in a Regional Healthcare System. Journal for the American College of Surgeons. DOI: https:/
1 Shah A, Hayes DJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use-United States 2006-2015. Morbidity and Mortality Weekly Report 2017. 66 (10): 265-269.
2 Appleby J, Lucas E. (2019, June 19) Surgeons’ Opioid-Prescribing Habits Are Hard to Kick, Kaiser Health News. Available at: https:/
About the American College of Surgeons
The American College of Surgeons is a scientific and educational organization of surgeons that was founded in 1913 to raise the standards of surgical practice and improve the quality of care for all surgical patients. The College is dedicated to the ethical and competent practice of surgery. Its achievements have significantly influenced the course of scientific surgery in America and have established it as an important advocate for all surgical patients. The College has more than 82,000 members and is the largest organization of surgeons in the world. For more information, visit http://www.
Media Contact
Sally Garneski
[email protected]
312-202-5409
Related Journal Article
http://dx.





