Lung cancer remains one of the most formidable adversaries in the realm of oncology. Its high mortality rates make it imperative to catch the disease early. One potential game changer in this battle against lung cancer is screening, a preventive healthcare measure aimed at detecting malignancies before they advance to later stages. However, the uptake of lung cancer screening in the United States has been disheartening; a study reveals that only 18% of eligible individuals take advantage of this life-saving opportunity. This statistic raises important questions about why so few eligible patients follow through with screening recommendations.
A recent study published in JAMA, spearheaded by researchers at Mass General Brigham, sheds light on this issue and challenges the prevailing assumption that a lack of interest in healthcare fuels low screening rates among eligible individuals. The researchers scrutinized data from the 2022 Behavioral Risk Factor Surveillance System dataset, which is maintained by the U.S. Centers for Disease Control and Prevention. They explored patterns of healthcare utilization among 28,483 individuals between the ages of 50 and 79, all of whom were eligible for lung cancer screening due to their smoking history.
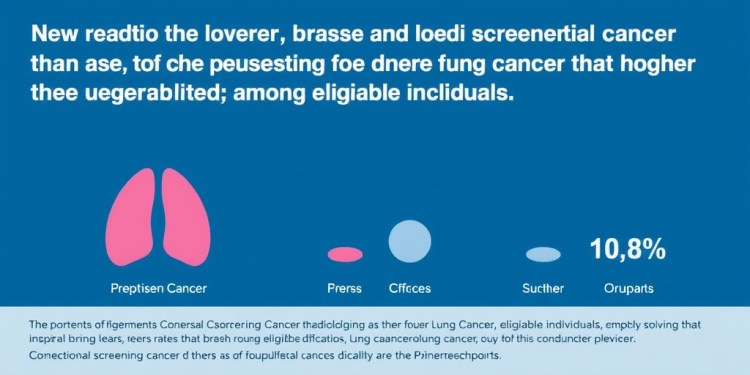
Astoundingly, while only 17-18% of this group opted for lung cancer screening, the same cohort demonstrated a much greater affinity for other forms of preventive care. Specifically, a striking 65% of those eligible for lung cancer screening also participated in breast and colorectal cancer screenings. This disparity suggests a level of engagement in preventive health services that contradicts the narrative of reluctance. The results insinuate that the issue lies not in the individuals themselves but rather in external barriers impacting their access to lung cancer screening.
First author Alexandra Potter, a dedicated researcher in the Division of Thoracic Surgery at Mass General Brigham, emphasized the importance of understanding the motivators behind these statistics. According to Potter, the data challenges the notion that eligible individuals are resistant to cancer screenings. Instead, she points towards a potentially complex interplay of factors that impede access to lung cancer screenings. Unlike breast and colorectal cancer screening, which rely mainly on age for eligibility, lung cancer screening criteria are notably intricate, factoring in both age and detailed smoking history. This complexity may confuse potential candidates, thereby impacting their willingness to pursue screening.
Beyond the maze of eligibility criteria, another dimension complicating the uptake of lung cancer screenings is accessibility. Potter’s research underscores that challenges related to accessing screening clinics could be significant barriers preventing high-risk individuals from engaging in lung cancer screening. The healthcare infrastructure currently in place may not adequately meet the needs of those at increased risk, further exacerbating the issue and marking a critical area of concern in public health.
As the researchers delved deeper into these dynamics, they concluded that many eligible individuals show a readiness to engage in preventive healthcare services, rejecting the notion that resistance is the primary culprit. Instead, they advocate for a broader awareness and understanding of lung cancer screening, emphasizing the importance of targeted interventions. Their findings present a clarion call for healthcare professionals, policymakers, and community leaders to enhance education around lung cancer screening.
In its current state, lung cancer diagnostic practices may be seen as archaic and inadequate, failing to catch up with advancements in public health strategies tailored for improving patient outcomes. Interventions should not only aim to educate but also reduce the barriers that keep high-risk individuals from the screenings they need. Collaborative community efforts could catalyze changes in awareness and accessibility, ultimately fostering an environment that better supports individuals seeking necessary healthcare services.
Conscientious steps must be taken to memorialize the importance of lung cancer screening in the national consciousness. Growing public understanding of this critical health service could drive increased participation, leading to earlier diagnoses and, consequently, improved outcomes. Researchers advocate a multifaceted approach that integrates ongoing education, simplified eligibility explanations, and improved clinic access to facilitate higher screening rates.
Additionally, the need for a comprehensive strategy that addresses both systemic barriers and individual motivations cannot be overstated. Empowering physicians to engage with individuals more meaningfully about their risks and the details surrounding lung cancer screenings could facilitate open dialogue. By fostering an atmosphere that prioritizes patient education, the hope is to enhance screening rates and, ultimately, save lives.
In summary, lung cancer screening is a vital component of cancer prevention that remains underutilized despite its proven efficacy. The recent research from Mass General Brigham paints a nuanced picture of the barriers faced by eligible populations, suggesting that low rates of participation are not merely a matter of personal choice. Addressing the complexities of eligibility criteria, clinic access, and public understanding are crucial steps in increasing screening rates among those most at risk.
Hence, as a community, it is essential for stakeholders across the spectrum of healthcare to work collaboratively. Engagement efforts that raise awareness of lung cancer screening and tailor interventions to reduce barriers could result in a significant impact on the lives of individuals at high risk of developing this deadly disease.
By acknowledging the multilevel factors that influence screening uptake, the future of lung cancer diagnosis and treatment may witness transformative changes that ultimately contribute to reduced mortality rates and improved patient outlooks in the fight against this menacing ailment.
Subject of Research: People
Article Title: Preventive Health Care Use Among Adults Eligible for Lung Cancer Screening in the US
News Publication Date: 2-Apr-2025
Web References: JAMA Article
References: 10.1001/jama.2025.2157
Image Credits: Mass General Brigham
Keywords: Lung cancer, Cancer screening, Disease prevention, Clinical research, Cancer research, Breast cancer, Colorectal cancer, Risk factors.
Tags: barriers to lung cancer screeningbreast cancer screening statisticscancer screening eligibility criteriacolorectal cancer screening comparisonhealthcare utilization patternshigh mortality rates of lung cancerJAMA cancer research findingslung cancer screening ratesMass General Brigham studypreventive healthcare measurespublic health and cancer preventionsmoking history and cancer risk