Credit: University of California Regents
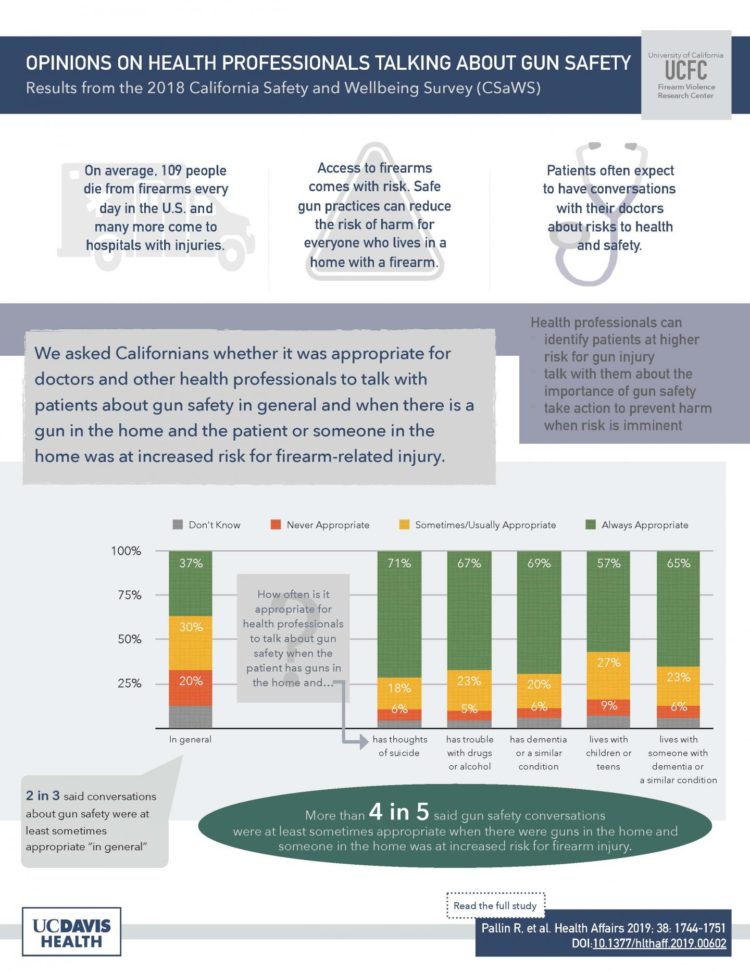
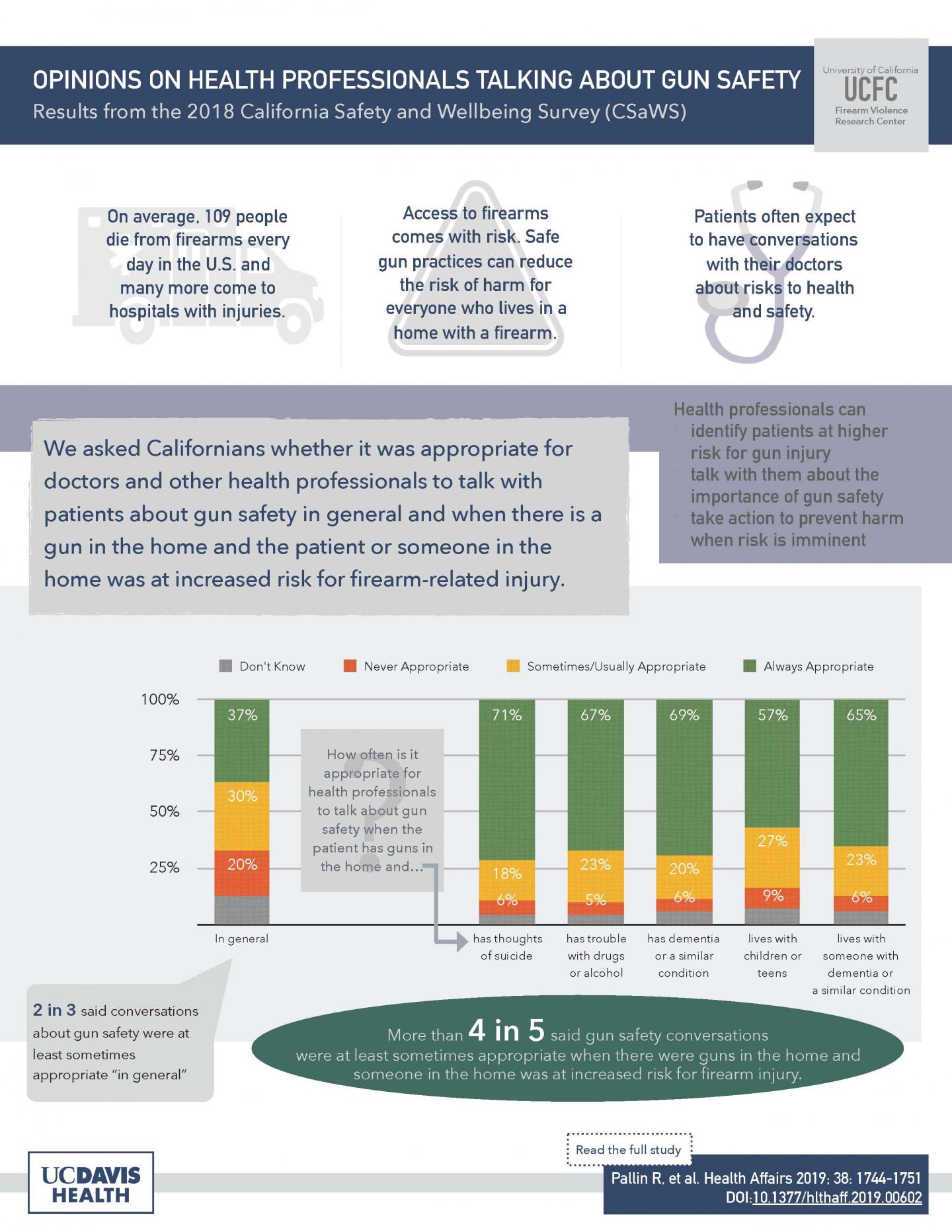
(SACRAMENTO, Calif.) — Most Californians find gun safety conversations that take place in the exam room appropriate if a patient has access to a gun and the patient — or someone in the patient’s home — is at increased risk for firearm-related harm, such as trouble with drugs or alcohol misuse.
That’s one of the main findings of a study by UC Davis researcher Rocco Pallin published Oct. 7 in Health Affairs‘ special issue on Violence and Health. While previous studies have found public support for health professionals talking with patients about gun safety in general, Pallin’s study is the first to ask about appropriateness of these conversations in specific risk scenarios.
Pallin will present her research at a news briefing on Thursday, October 10 in Washington, D.C. (register to attend in person or via webcast). The survey is one of three studies by UC Davis researchers published in the Health Affairs special issue.
“Health care providers have unique potential to recognize risk for firearm injury and — when risk is elevated and there’s access to a gun — to talk with patients about safe gun practices,” Pallin said. “But providers infrequently assess risk and engage with patients in these conversations in part because they think patients won’t be receptive or that such discussions may alienate them. Our results suggest that these conversations are broadly acceptable, and that patients may find them most appropriate when there is specific risk.”
Over the past 10 years ending in 2017, fatalities from firearm violence among civilians in the U.S. exceeded combat fatalities in World War II. Firearm homicides have increased by 32% since 2014, suicides by 41% since 2006 and the number of nonfatal crime victims by 37% since 2013.
Talking about gun safety: gun owners vs. non-owners
Forty percent of gun owners in the study sample reported that gun safety conversations were never appropriate in general, compared with less than 20% of those who did not own guns. Given scenarios in which risk for firearm-related harm was elevated, however, few differences existed between gun owners and non-owners, and support for these conversations was high.
“We saw little variation in support for gun safety conversations between those who own guns and those who don’t when someone was at increased risk,” said Pallin. “This lends support to the current recommendation that providers take a risk-based approach to talking about gun safety rather than universally counseling their patients.”
The largest difference in support was in response to a patient with access to a gun and living with children or teens: fewer gun owners (70%) found this an appropriate scenario for a gun safety conversation compared with non-owners (87%). The authors cite research that shows children and teens are at increased risk for accidental firearm injury and suicide when guns are in the home. They say this finding suggests that the public may not fully appreciate the risks for children and teens, which may have clinical implications for pediatricians who speak with parents about gun safety.
Interventions for patients at acute risk
Four out of five respondents, regardless of gun ownership status, said it was at least sometimes appropriate for a doctor to intervene to reduce firearm injury when a patient with access to a gun had thoughts of self-harm or harming others. Suggested interventions included counseling the patient to have someone else keep the gun and informing the patient’s family.
This study is the first to gauge public opinion on the appropriateness of temporary transfer when someone with access to a gun is in crisis. The high level of support for this intervention, regardless of firearm ownership status, suggests this may be a reasonable risk reduction strategy, Pallin said.
“When someone is suicidal, reducing access to lethal means can be lifesaving, and temporary transfer is one option,” she explained. The authors recommend that providers be informed about relevant statutes, which vary by state, in order to make lawful and realistic recommendations.
Increased attention has been given to the role of health care providers in reducing firearm injuries in the last two years, but Pallin suggests more work needs to be done.
“Clinicians, firearm owners, safety instructors and researchers need to work together to develop and evaluate approaches to assess patient risk, counseling on gun safety when clinically relevant, and intervening in emergency situations. We need to understand what works best for certain types of risk, certain types of providers, and certain types of patients in order to educate providers to most effectively and efficiently work to prevent firearm-related harm,” she said. The state of California recently appropriated funds to develop clinician training on strategies for firearm injury prevention, which has the potential to become a national model.
For the study, UC Davis researchers analyzed data from the 2018 California Safety and Wellbeing Survey (CSaWS). The comprehensive, online survey is conducted annually to gather information and opinions on a wide range of topics related to firearm ownership. It included responses from more than 2,500 Californians ages 18 and older and yields state-representative estimates.
###
Co-authors of the study “California public opinion on health professionals talking with patients about firearms” include Amanda Charbonneau, Garen J. Wintemute and Nicole Kravitz-Wirtz, all of UC Davis Health. A brief of the study is also available online.
This research was supported by the University of California Firearm Violence Research Center with funds from the State of California. Additional support came from the California Wellness Foundation (Award No. 2014-255), the Heising-Simons Foundation (Award No. 2017-0447), the Langeloth Foundation (Award No. 1824), and the University of California Davis Violence Prevention Research Program.
The UC Davis Violence Prevention Research Program (VPRP) is a multi-disciplinary program of research and policy development focused on the causes, consequences and prevention of violence. Studies assess firearm violence and the connections between violence, substance abuse and mental illness. VPRP is home to the University of California Firearm Violence Research Center, launched in 2017 with an appropriation from the state of California.
Media Contact
Carole Gan
[email protected]
916-734-9047
Original Source
https:/
Related Journal Article
http://dx.