Macrophages, a type of white blood cell that can destroy invading pathogens, have an innate ability to infiltrate tumor cells, making them a potentially important tool in treatments that use transplanted cells to fight disease, known as cell therapy. In the lab, macrophages show a lot of promise in treating cancer but so far, clinical trials have been a disappointment and biologists are trying to figure out why.
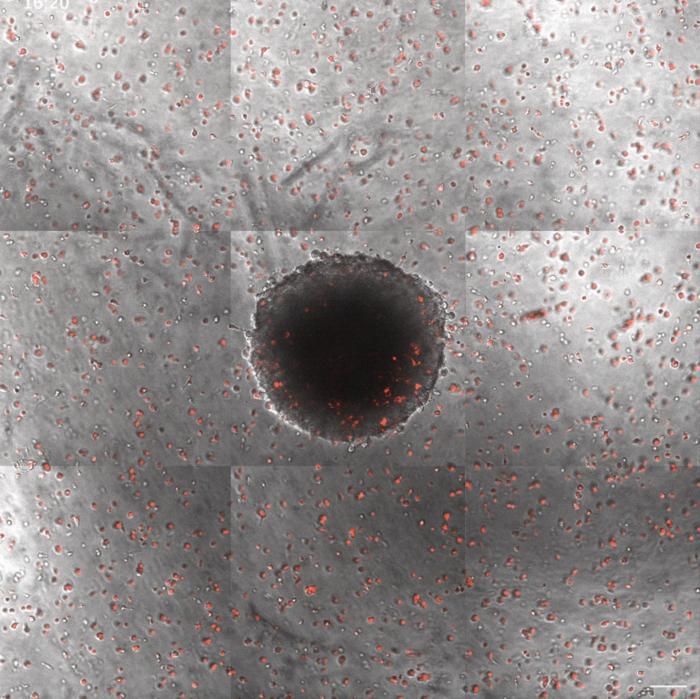
Credit: (Credit: The Mitragotri Laboratory for Drug Delivery/Harvard SEAS)
Macrophages, a type of white blood cell that can destroy invading pathogens, have an innate ability to infiltrate tumor cells, making them a potentially important tool in treatments that use transplanted cells to fight disease, known as cell therapy. In the lab, macrophages show a lot of promise in treating cancer but so far, clinical trials have been a disappointment and biologists are trying to figure out why.
But what if it’s not a biological problem?
In a recent paper, researchers from the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) approached the failure of macrophages in clinical trials from an engineering perspective.
The research team, led by Samir Mitragotri, the Hiller Professor of Bioengineering and Hansjorg Wyss Professor of Biologically Inspired Engineering at SEAS, looked at the physical barriers that might be preventing macrophages from reaching their target in the first place.
By combining microscopy with machine learning, the team found that a specific phenotype of macrophage was better at traveling to the tumor than others — and it’s not the one that researchers commonly use in the clinic for cancer therapies.
The research was published Applied Physics Reviews.
“Our engineering approach led us to question whether the poor therapeutic outcome of macrophages in cell therapies can in part originate from their inability to get into the tumor in the first place,” said Mitragotri. “And indeed, our results show that different phenotypes exhibit different penetration into the tumor. This provides an interesting physics-based hypothesis for the poor clinical outcome of previously reported macrophage therapies and provides a counter- and complimentary hypothesis to the classical biology-based paradigm.”
There are multiple types of macrophages, simplified as M0, M1, and M2. Of the three, M1 macrophages have the best tumor-fighting capacities and therefore have been used the most for cell therapies. But they have yielded disappointing results in clinical trials.
Mitragotri and his team looked at how each of the three different phenotypes could move through a complex hydrogel and into a tumor in a petri dish.
“We basically wanted to measure how well the transport mechanics and GPS of these different macrophages worked in a complex environment,” said Kolade Adebowale, a postdoctoral fellow at SEAS and first author of the paper. “We found that the M1 phenotype, anti-tumor microphage, seem to have trouble finding their targets, almost like their GPS wasn’t working. But the M0 phenotype seemed to have a really good map.”
The big question is why.
It’s well known that macrophages exist in various shapes and some phenotypes are really good at changing their shape. Adebowale and the team found a correlation between shape-shifting abilities and transport efficiency — meaning the better the macrophage was at shape shifting, the better able they were to get to the tumor.
And, as it turned out, M1 macrophages are the worst of the three when it comes to shapeshifting.
“Our study demonstrates that the reduced transport of M1 macrophages compared to M0 macrophages is correlated with their reduced ability to undergo shape transformations,” said Adebowale. “We hope that these findings shed new light on the biophysics of macrophage migration and delivery of macrophage cell therapies.”
“There is tremendous potential in utilizing macrophages to mediate anti-tumor immune responses in human tumors and clinical trials are ongoing to treat patients with macrophages,” said Jennifer Guerriero, Assistant Professor at Harvard Medical School, lead investigator of Brigham and Women’s Hospital Breast Oncology Program and co-author of the study. “We learned in this study that, surprisingly, macrophages that resemble an M0 phenotype were most efficient at getting to their target. These data will have an immediate impact on clinical trials are likely to transform the next generation of macrophage-mediated therapies.”
The research was supported by the National Science Foundation under Award No. 2138064.
Journal
Applied Physics Reviews
DOI
10.1063/5.0160924



