Penn brain imaging study finds negative implicit biases against individuals with scars, birthmarks and other facial differences
Credit: Penn Medicine
PHILADELPHIA–People with attractive faces are often seen as more trustworthy, socially competent, better adjusted, and more capable in school and work. The correlation of attractiveness and positive character traits leads to a “beautiful is good” stereotype. However, little has been understood about the behavioral and neural responses to those with facial abnormalities, such as scars, skin cancers, birthmarks, and other disfigurements. A new study led by Penn Medicine researchers, which published today in Scientific Reports, uncovered an automatic “disfigured is bad” bias that also exists in contrast to “beautiful is good.”
“Judgements on attractiveness and trustworthiness are consistent across cultures, and these assumptions based on facial beauty are made extremely quickly. On the other hand, people with facial disfigurement are often targets of discrimination, which seems to extend beyond the specific effects of lower overall attractiveness and may tie in more with the pattern of results with stigmatized groups,” said the study’s lead author Anjan Chatterjee, MD, a professor of Neurology, and director of the Penn Center for Neuroaesthetics. “In order to right any discrimination, the first step is to understand how and why such biases exist, which is why we set out to uncover the neural responses to disfigured faces.”
Neuroimaging studies show that seeing attractive faces evokes brain responses in reward, emotion, and visual areas compared to seeing faces of average attractiveness. Specifically, attractive faces evoke greater neural responses as compared to faces of average attractiveness in ventral occipito-temporal cortical areas, which process faces and other objects. Additionally, attractiveness correlates with increased activations in the anterior cingulate cortex and medial-prefrontal cortex–areas which are associated with rewards, empathy, and social cognition.
The researchers set out to evaluate the behavioral and brain reactions to disfigured faces and investigate whether surgical treatment mitigates these responses. In two experiments, the researchers used a set of photographs of patients with different types of facial anomalies, before and after surgical treatment, to test whether people harbor a “disfigured is bad” bias and to measure neural responses.
In the first experiment, a behavioral study with 79 participants, the researchers tested if people harbor implicit biases against disfigured faces and if such implicit biases were different from consciously aware, self-reported explicit biases. The behavioral experiment consisted of an implicit association test (IAT) and an explicit bias questionnaire (EBQ) to identify whether people have a negative bias for disfigured faces. For the IAT, the researchers used the set of before and after photographs as a stimulus. The EBQ consisted of 11 questions which query conscious biases against people with facial disfigurements. While the team found no indication of an explicit bias, they found that non-disfigured faces were preferred in the IAT. This bias was particularly robust for men.
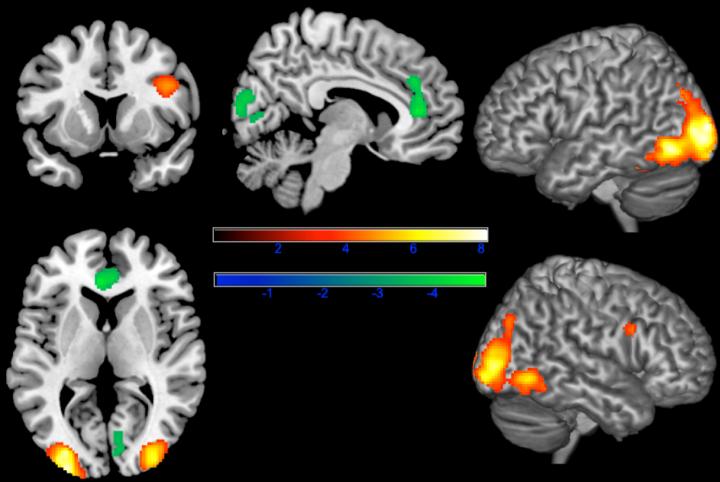
In a follow up functional MRI (fMRI) study with 31 participants, researchers tested brain responses to the same picture pairs. Participants judged the gender of each photograph they viewed. The researchers found increased neural responses in visual regions of the brain (the ventral occipito-temporal cortical areas) and decreases in regions associated with empathy (the anterior cingulate and medio-prefrontal cortex).
In sum, the authors found that people have implicit negative biases against people with disfigured faces, without knowingly harboring such biases. The diminished neural responses in the anterior cingulate cortex suggests that people are less empathetic when looking at individuals with disfigurement–this is also a potential neural marker of dehumanization, as diminished neural responses in the anterior cingulate cortex is also observed in response to other stigmatized people, such as the homeless and drug addicts.
“The emphasis of attractiveness and its association with positive attributes highlights the pervasive effect of appearance in social interaction. Chatterjee said. “While we found that corrective surgery mitigates negative social and psychological responses to people with facial anomalies, we are also exploring alternative strategies to minimize bias towards people with facial conditions.”
###
This work was supported by the Penn Center for Human Appearance and the Global Wellness Institute.
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation’s first medical school) and the University of Pennsylvania Health System, which together form a $7.8 billion enterprise.
The Perelman School of Medicine has been ranked among the top medical schools in the United States for more than 20 years, according to U.S. News & World Report’s survey of research-oriented medical schools. The School is consistently among the nation’s top recipients of funding from the National Institutes of Health, with $425 million awarded in the 2018 fiscal year.
The University of Pennsylvania Health System’s patient care facilities include: the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center–which are recognized as one of the nation’s top “Honor Roll” hospitals by U.S. News & World Report–Chester County Hospital; Lancaster General Health; Penn Medicine Princeton Health; and Pennsylvania Hospital, the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Home Care and Hospice Services, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is powered by a talented and dedicated workforce of more than 40,000 people. The organization also has alliances with top community health systems across both Southeastern Pennsylvania and Southern New Jersey, creating more options for patients no matter where they live.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2018, Penn Medicine provided more than $525 million to benefit our community.
Media Contact
Hannah Messinger
[email protected]
Original Source
https:/
Related Journal Article
http://dx.




